Hospitals and specialist centres are complex by design. Multiple storeys, interconnected wings, pop-up clinics, evolving services, and a changing cast of clinicians create a living environment that is notoriously difficult to navigate—even for regular visitors. For patients and families, that complexity often collides with moments of anxiety or vulnerability. For staff, daily interruptions to give directions erode time that could be spent on care.
Digital wayfinding bridges these realities. It transforms how people find their way, turning intricate facilities into intuitive journeys. Done well, it is not simply a map on a screen—it is an inclusive, accessible guidance system that anticipates needs, adapts to change, and orchestrates a better experience from the car park to the clinic and back again.
What is digital wayfinding in healthcare?
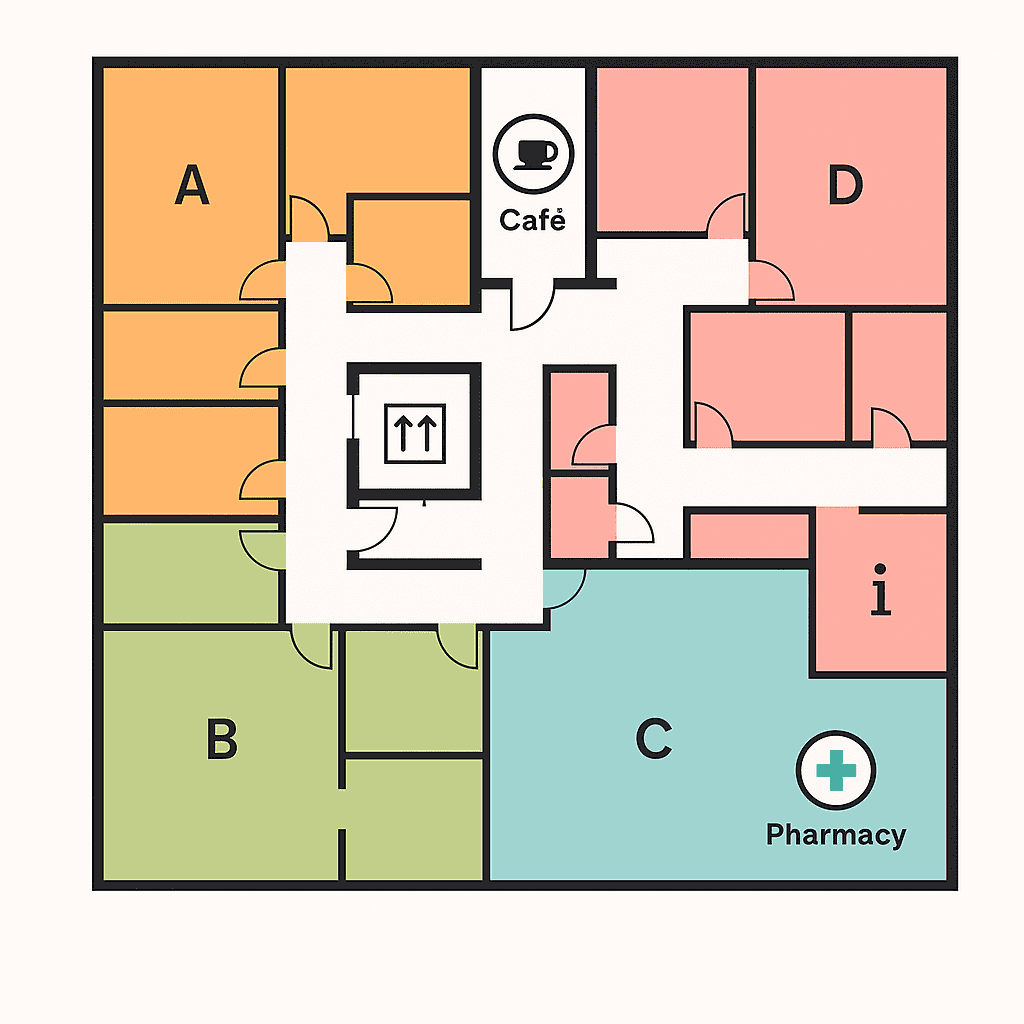
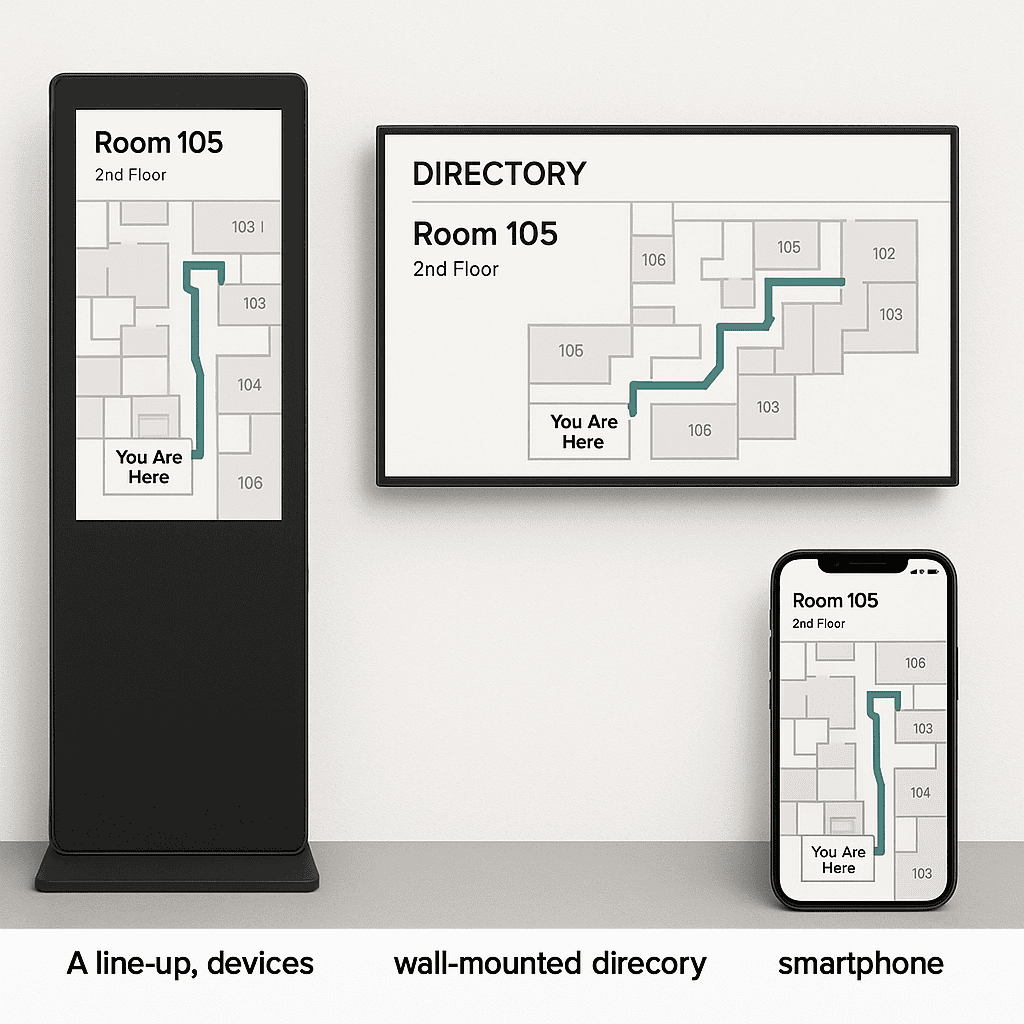
Digital wayfinding is a blend of mapping, signage, content, and technology that helps people orient themselves and navigate to their destination. In medical settings, it usually comprises interactive kiosks, mobile-friendly maps, digital directory boards, and dynamic signage that update in real time. Crucially, it integrates with clinic directories, appointment systems, and operational data (such as lift outages or construction), so routes stay reliable and step-free when needed.
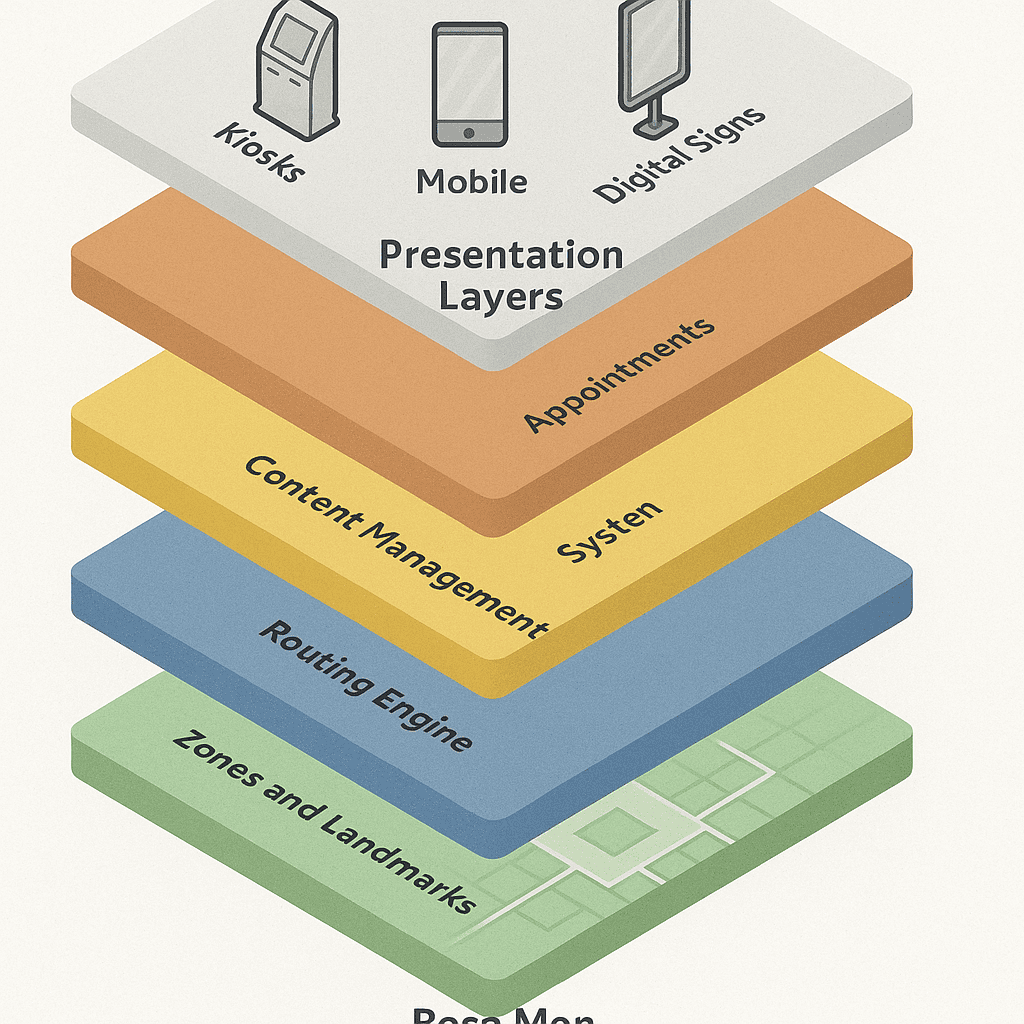
Think of it as a layered system:
- Strategy and taxonomy: a structured set of names, zones, destinations, and sign types that are consistent across print and digital.
- Content and design: clear maps, icons, colours, and language that are inclusive and understandable.
- Technology: the hardware (kiosks, screens), software (maps, search, routing, CMS), and integrations (scheduling, parking, accessibility) that make it dynamic.
- Operations: governance, workflows, monitoring, and maintenance that keep everything current and dependable.
Why medical centres benefit from digital wayfinding
Most health campuses grow over time. Corridors get extended, new wings are attached, departments move, and signage accrues like sediment. Static signs alone cannot keep pace. Digital wayfinding complements your signage programme with adaptive guidance, unlocking benefits across experience, safety, and efficiency:
- Reduced stress and anxiety: clear, step-by-step routes lower the cognitive load during already stressful visits.
- Improved punctuality: reliable routes, parking guidance, and realistic walk times reduce late arrivals and missed appointments.
- Staff time saved: fewer interruptions at reception and in corridors; staff can direct patients to kiosks or share a link with a route.
- Rapid updates: closures, detours, new clinics, or temporary relocations can be reflected instantly across all screens.
- Inclusive access: interfaces designed for different languages, abilities, and literacy levels help everyone find care.
- Consistent information: unified naming and zoning across digital and static signage avoid conflicting directions.
- Data-driven improvement: anonymous analytics reveal search trends and bottlenecks to inform service design.
- Sustainability: fewer reprints of floor plans and directional leaflets; dynamic signage reduces waste.
- Brand experience: a coherent visual system communicates competence, care, and attention to detail.
- Resilience: emergency messages and operational notices can appear instantly on relevant screens.
Map the patient journey, not just the building
Every medical centre serves multiple journeys: outpatient appointments, diagnostic imaging, pathology, day surgery, allied health, maternity, child health, oncology, and more. Each journey has its own stress points and information needs. Digital wayfinding should be designed around these journeys, not merely around corridors.
Pre-visit
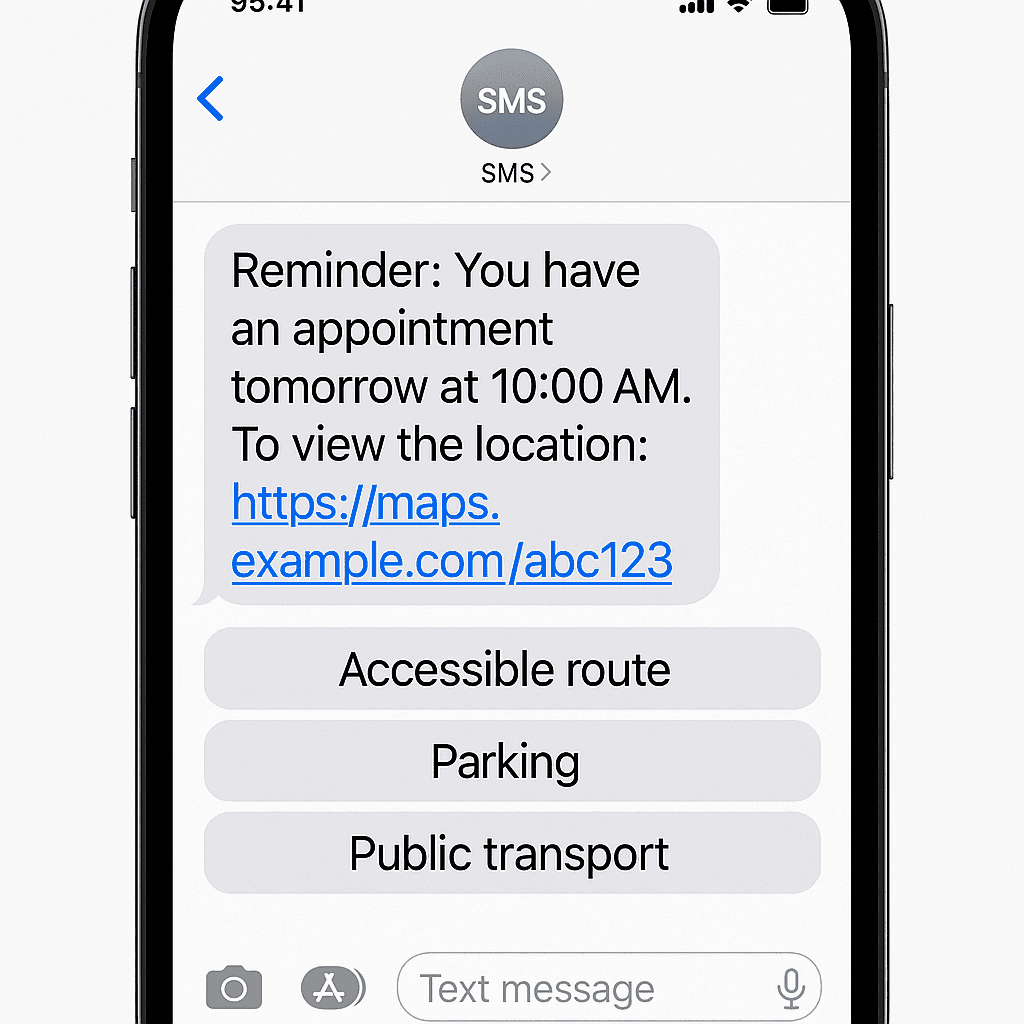
- Appointment reminders include a personalised link: “Plan your route to Cardiology, Level 3, Zone C.”
- Web maps present travel options, accessible parking, drop-off points, and estimated walk times.
- QR codes on appointment letters resolve to the right destination, not just a homepage.
Arrival and parking
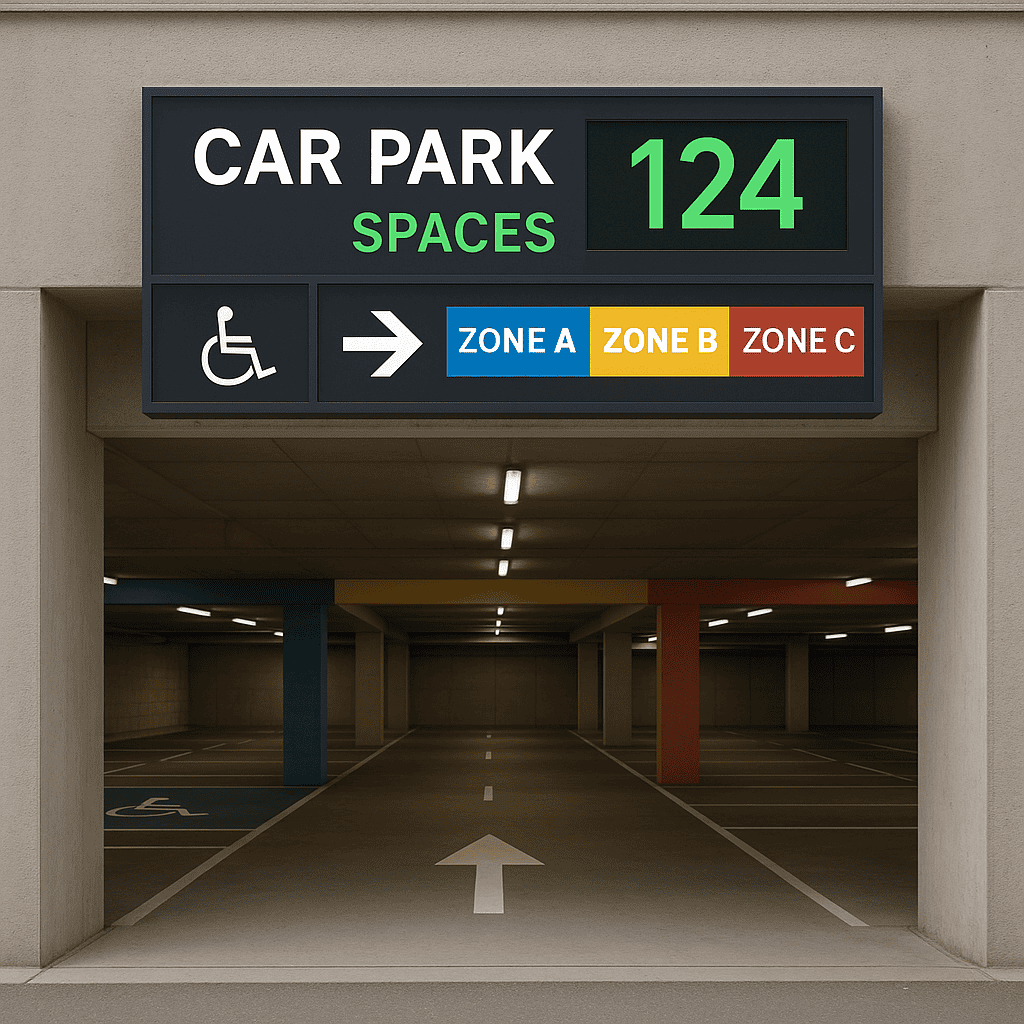
- Dynamic parking information helps visitors choose the best car park with real-time occupancy where available.
- Wayfinding starts at the perimeter: entrances, drop-off zones, and the most suitable entry for the destination.
- Accessible bays, lift cores, and ramped entries are explicitly highlighted.
Inside the building
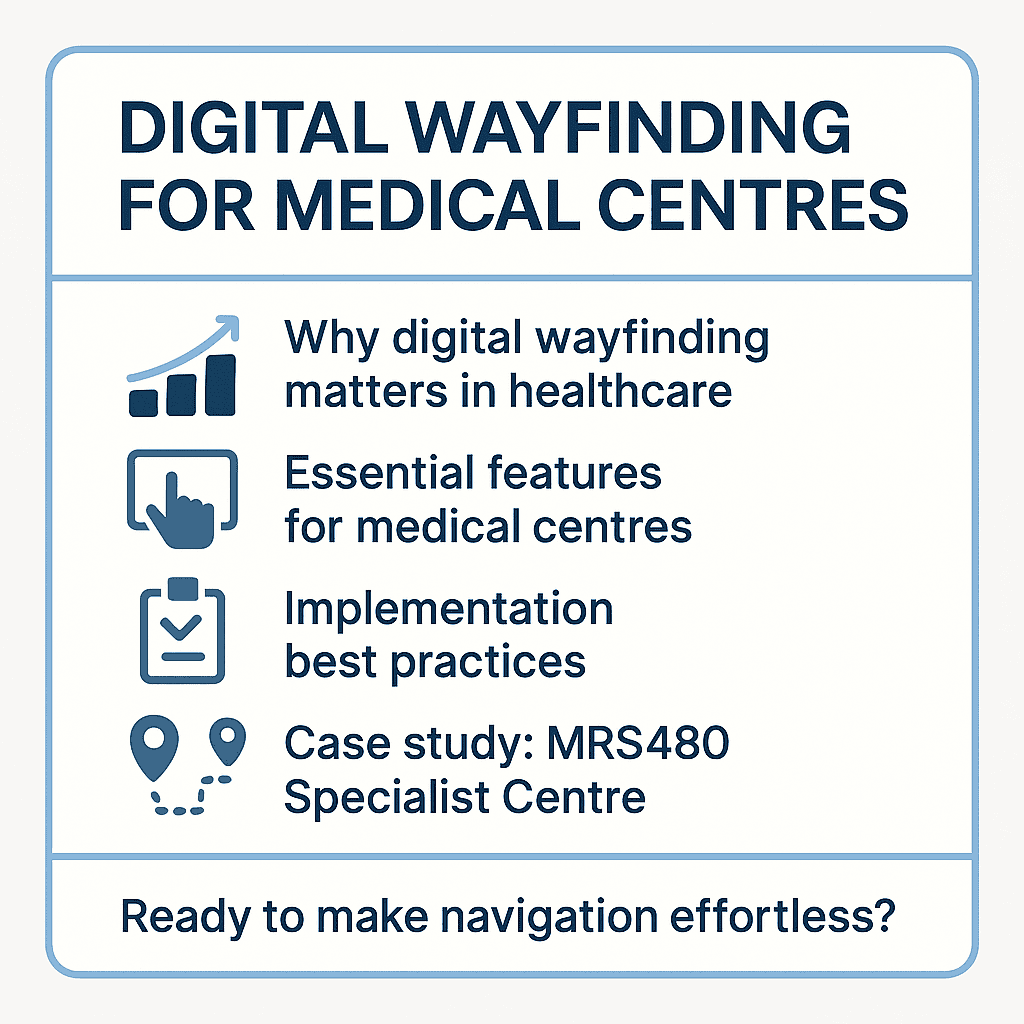
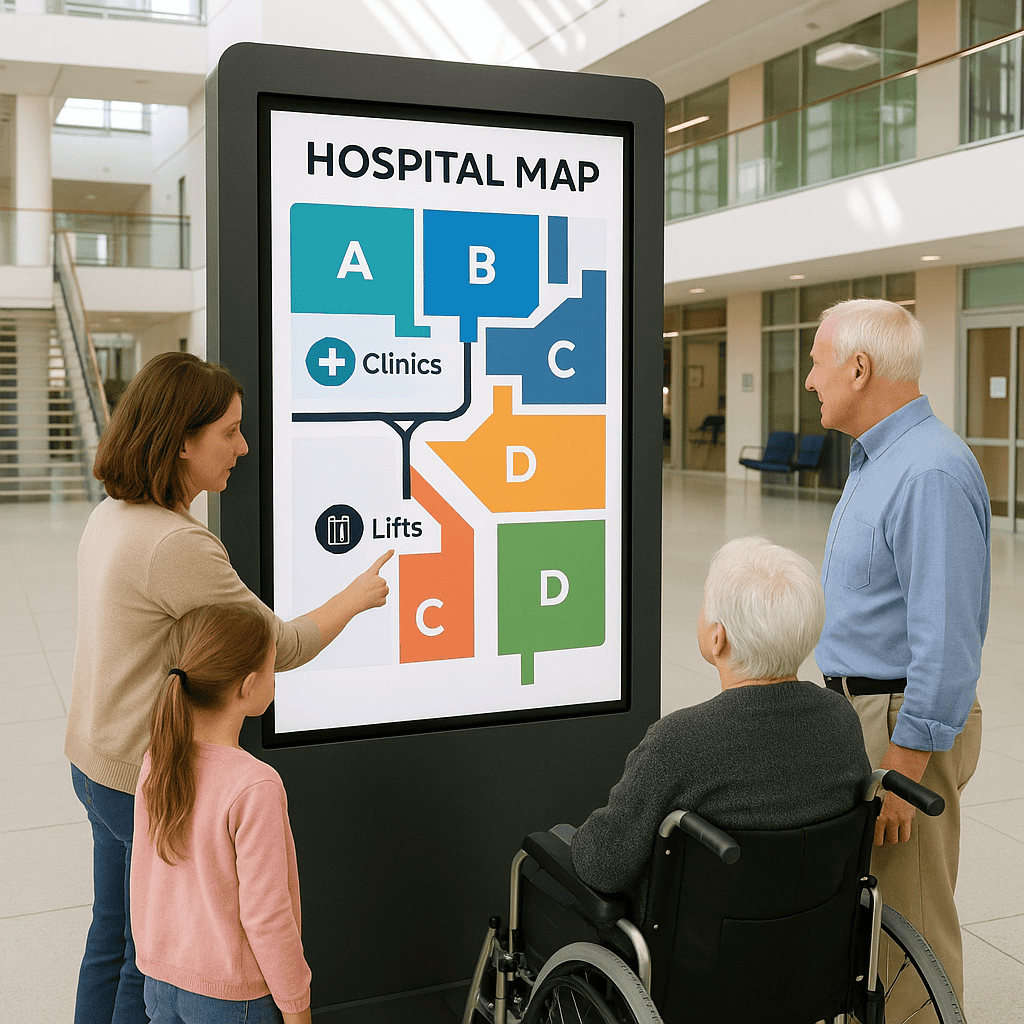
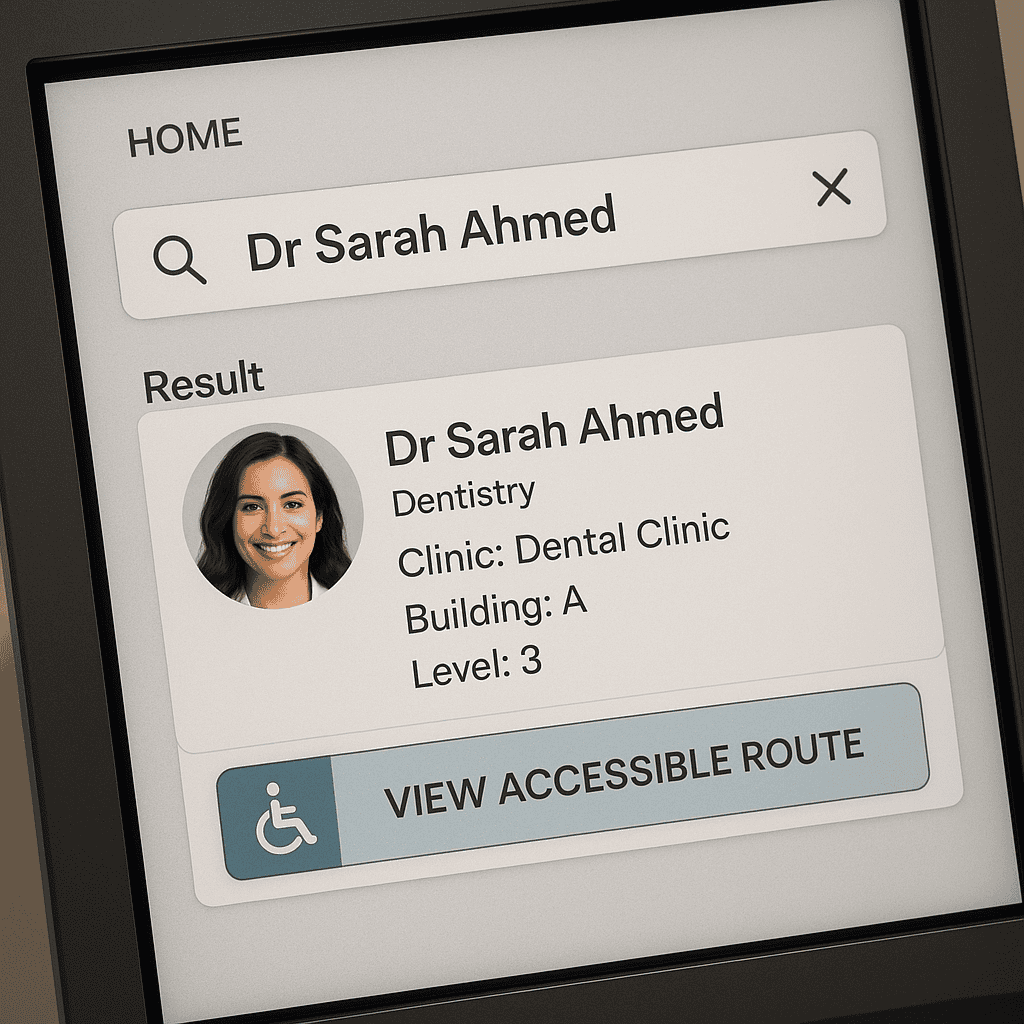
- Interactive kiosks in lobbies and key decision points provide search by clinician name, specialty, clinic, or procedure.
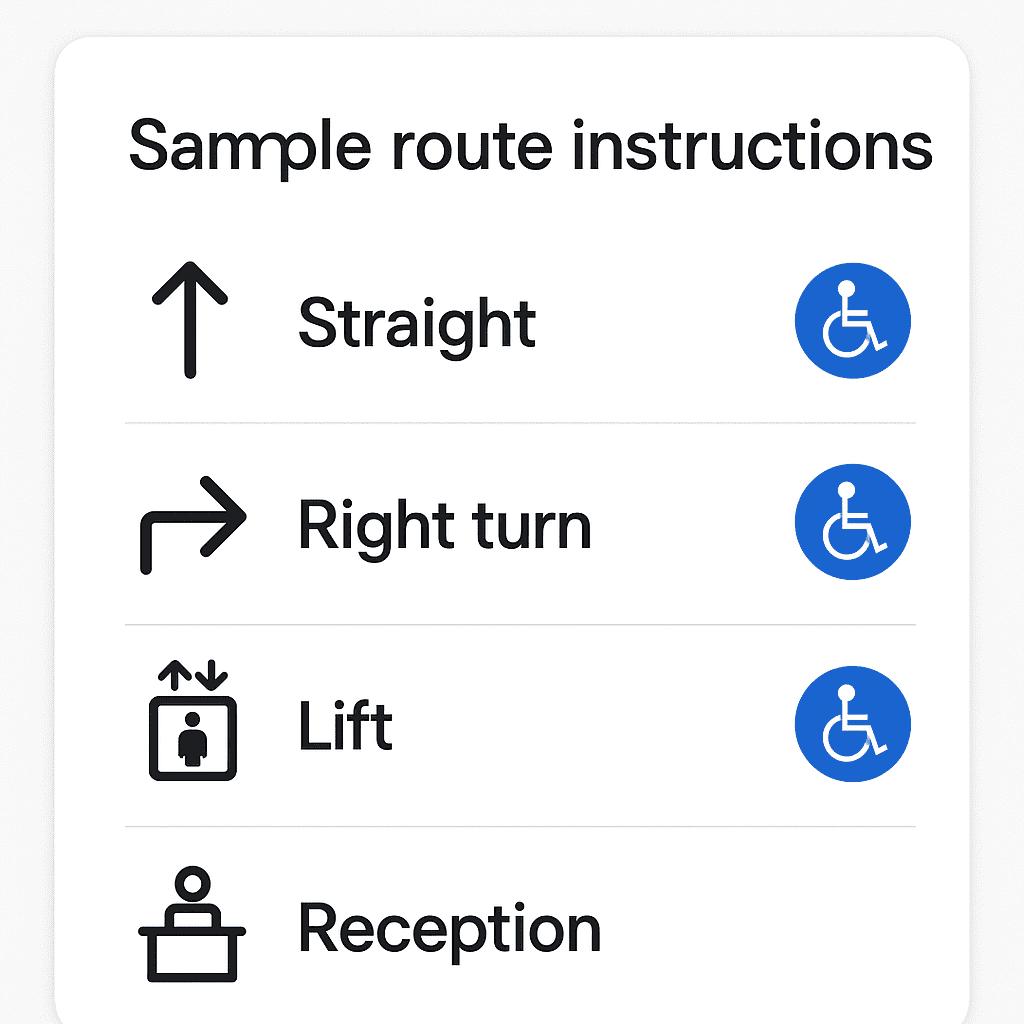
- Step-by-step routes support step-free navigation, clearly indicating lifts, rest points, and amenities.
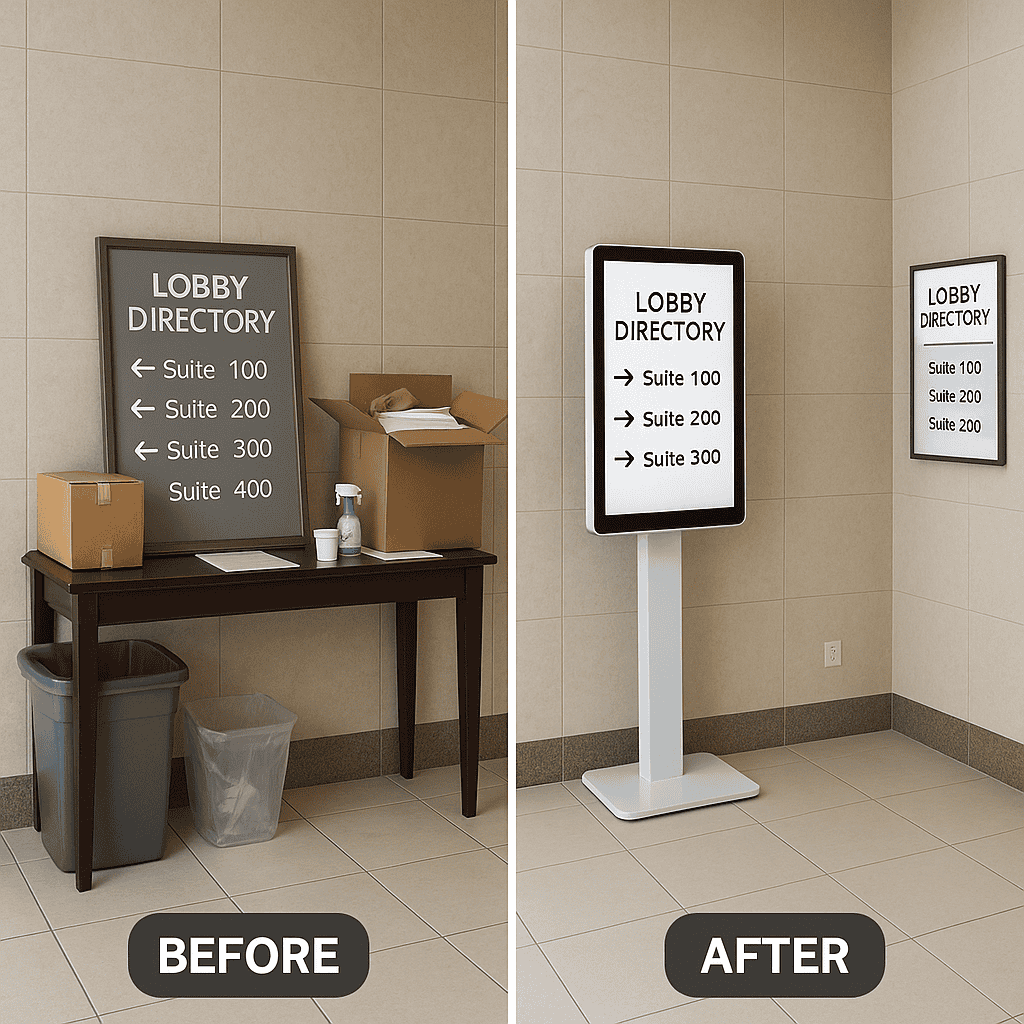
- Digital directory boards guide people to the right lift bank and storey; secondary screens reinforce decision points.
During the visit
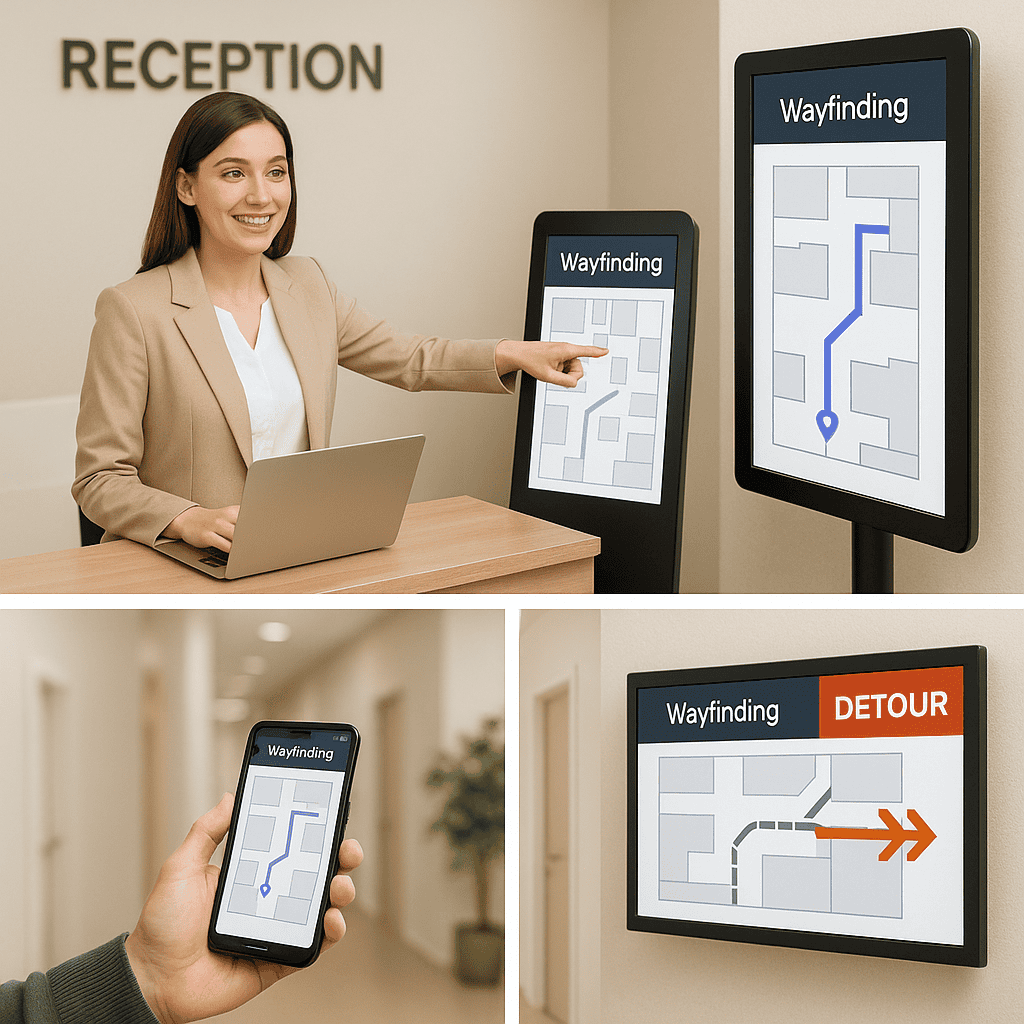
- Changes to clinic location, temporary closures, or detours update instantly across maps and signs.
- Queue and appointment systems can sync to show “Proceed to Radiology Reception B” on the visitor’s phone.
- Amenities such as toilets, café, pharmacy, and baby change rooms are included in wayfinding results.
Departure and beyond
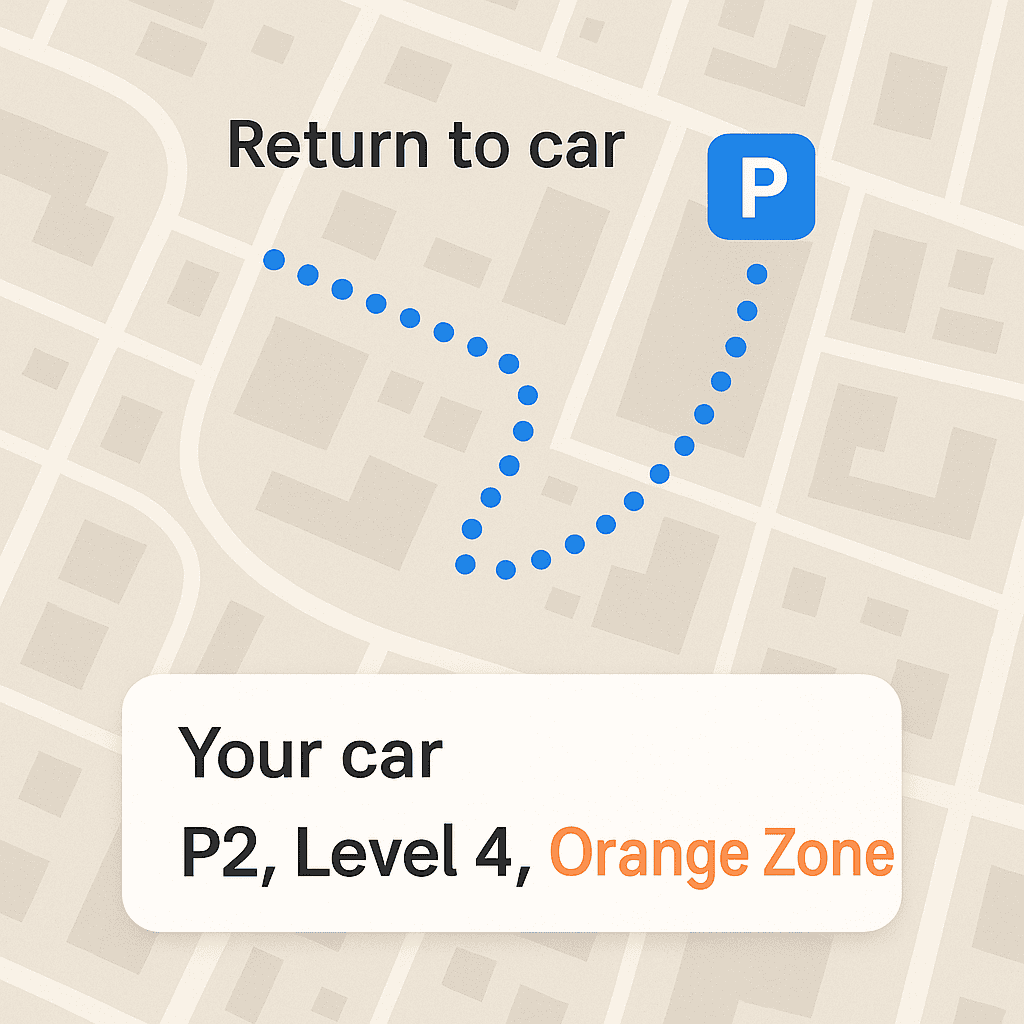
- Routes back to the car park with reminders of the level and colour zone where the car was parked.
- Links to pay for parking, request a wheelchair escort, or find the nearest taxi rank.
- Patient feedback prompts: “Was this route helpful?” to support continuous improvement.
Accessibility and inclusion: bake it in, don’t bolt it on
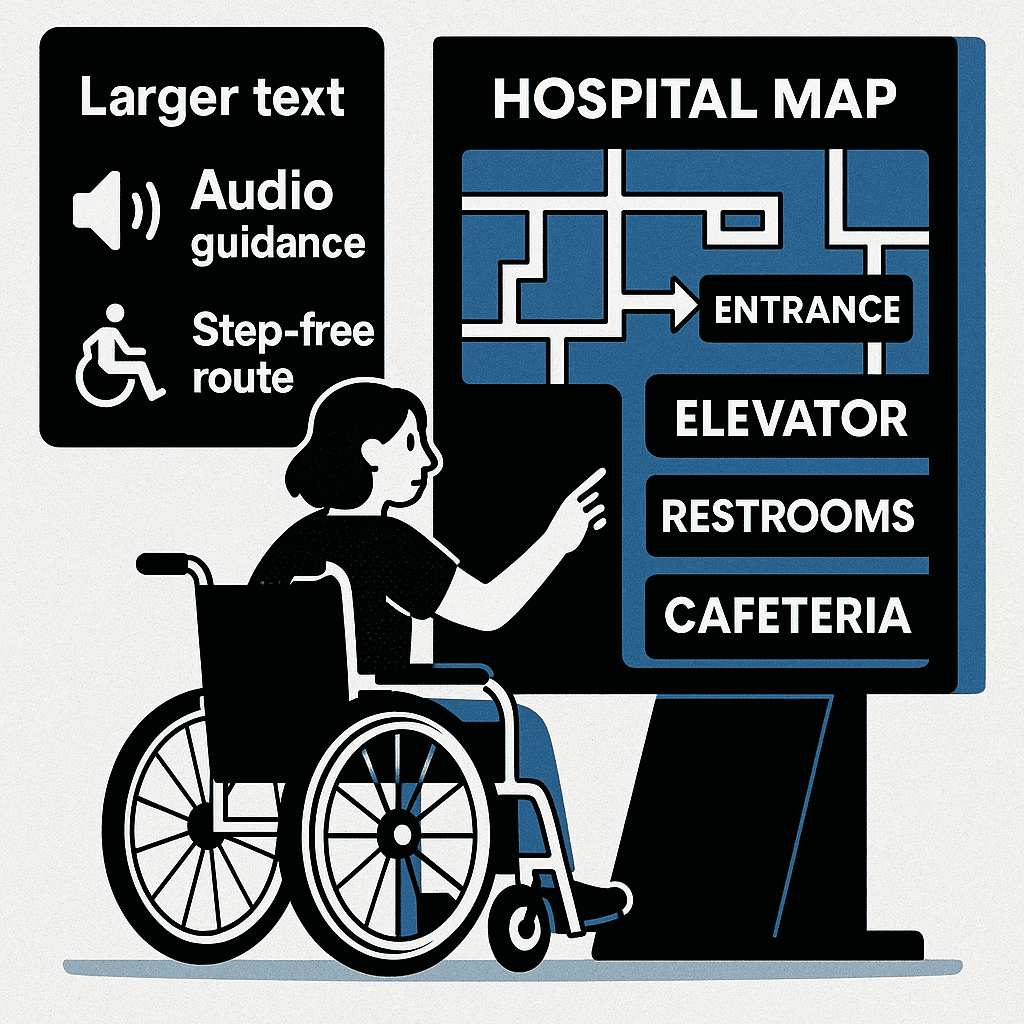
Healthcare serves everyone. Digital wayfinding must be usable by people with diverse abilities, languages, and literacy levels. Accessibility is not a feature; it is fundamental. Consider the following:
Standards and principles
- Design interfaces to meet or exceed WCAG 2.2 AA for contrast, text size, operability, and non-text alternatives.
- Follow Australian accessibility and building standards, such as AS 1428 for access and mobility, in your physical and digital wayfinding strategy.
- Ensure consistent naming and iconography across print and digital so that cues are reinforced in every medium.
Inclusive interface features
- Large touch targets and generous spacing to support tremors or limited dexterity.
- High-contrast colour palette with a minimum contrast ratio that maintains legibility in bright lobbies.
- Dynamic type scaling and “increase text size” toggle for kiosks and mobile.
- Text-to-speech (on-device where possible) with clear voice prompts and headphone support.
- Multiple languages based on local community needs; use culturally sensitive phrasing and images.
- Clear, plain English labels, avoiding clinical jargon; include synonyms (“Medical Imaging” and “Radiology”).
- Step-free routing as a default option; explicit indication of stairs, ramps, gradients, and lift locations.
Designing for cognitive load and stress
- Use progressive disclosure: reveal complexity only as needed; start with a simple journey overview.
- Provide landmarks in directions: “Pass the café” or “After the art wall, turn right.”
- Use a predictable colour-coded zoning system across all floors and signs.
- Offer calm-mode visuals with reduced motion, fewer animations, and muted transitions.
Consider specific populations
- Older adults: bigger text, stronger contrast, fewer steps per screen, and seats/rest points along routes.
- Paediatric settings: friendlier iconography, parent-focused instructions, and distraction minimised near clinical areas.
- Dementia-friendly: simple decision points, minimal branching, consistent cues, and avoidance of visual clutter.
- Neurodiverse users: clear sequencing, consistency, and user control over information density.
Designing a healthcare wayfinding system: from taxonomy to typography
A strong digital wayfinding programme starts with a robust information architecture and visual system. Map-first thinking is essential, but the map is supported by consistent naming and signage logic:
Destination taxonomy
- Establish a canonical list of destinations: clinics, departments, reception desks, procedures, amenities.
- Define relationships and synonyms (e.g., “Gynaecology” and “Women’s Health” point to the same destination).
- Store metadata for each destination: building, level, zone, lift bank, opening hours, phone, and step-free status.
- Handle temporary destinations (e.g., pop-up vaccination clinic) with start/end dates and automatic sunset.
Zoning and landmarks
- Create colour-coded zones with names that are easy to say and remember; avoid non-intuitive numbering jumps.
- Assign notable, permanent landmarks to anchor directions: café, sculpture, information desk, garden.
- Mark decision points (lift lobbies, corridors) clearly; reinforce zones at each key decision point.
Typography and iconography
- Use a legible humanist sans-serif typeface optimised for large and small sizes; avoid condensed faces.
- Develop an icon set that is consistent and tested for comprehension; avoid ambiguous metaphors.
- Ensure text and icons maintain legibility from typical viewing distances in lobbies and corridors.
Language and messaging
- Write in plain English; prefer “go to the lift” over “proceed to the vertical circulation core.”
- Use short verbs and active voice; avoid medical abbreviations unless commonly understood.
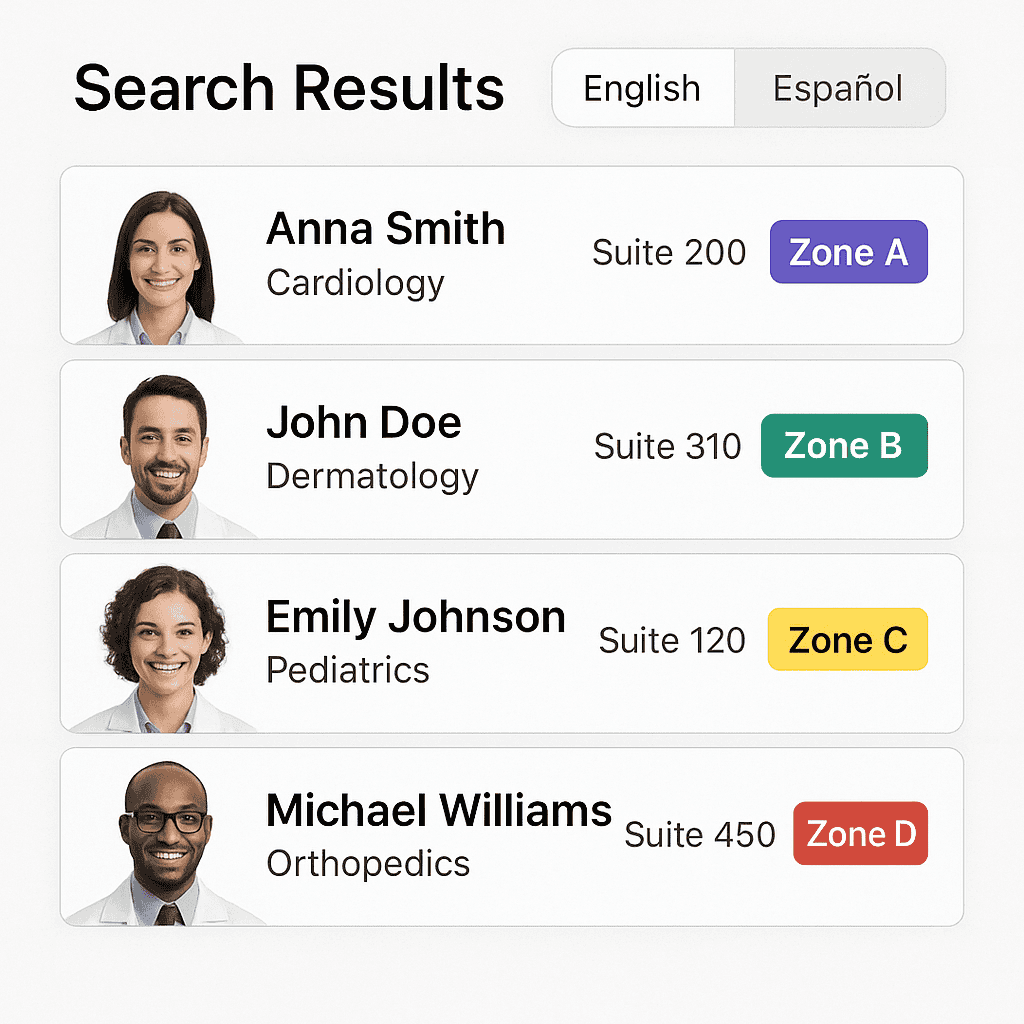
- Handle names with care: clearly present clinician names, specialties, and consulting suite numbers.
Consistency between physical and digital
- Digital routes must match physical signage naming, colours, and codes.
- Static signs should include QR codes to “continue the route on your phone.”
- Align map orientation to the user’s perspective at kiosks (“you are here” facing forward), but allow north-up on mobile.
Technology options and how to choose them
There is no one-size-fits-all. The right mix of screens, positioning technologies, and integrations depends on your building fabric, budget, and journeys. Below are the essentials and optional enhancements.
Core presentation channels
- Interactive kiosks: portrait touchscreens in lobbies and decision points, in secure kiosk mode with antimicrobial glass.
- Digital directory boards: non-touch, large-format displays listing clinics, rooms, and directional prompts.
- Mobile web: responsive, app-free maps with deep links from emails/SMS and QR codes on signage.
- Printed takeaways: optional “print or save your route” slips with QR codes to resume on mobile.
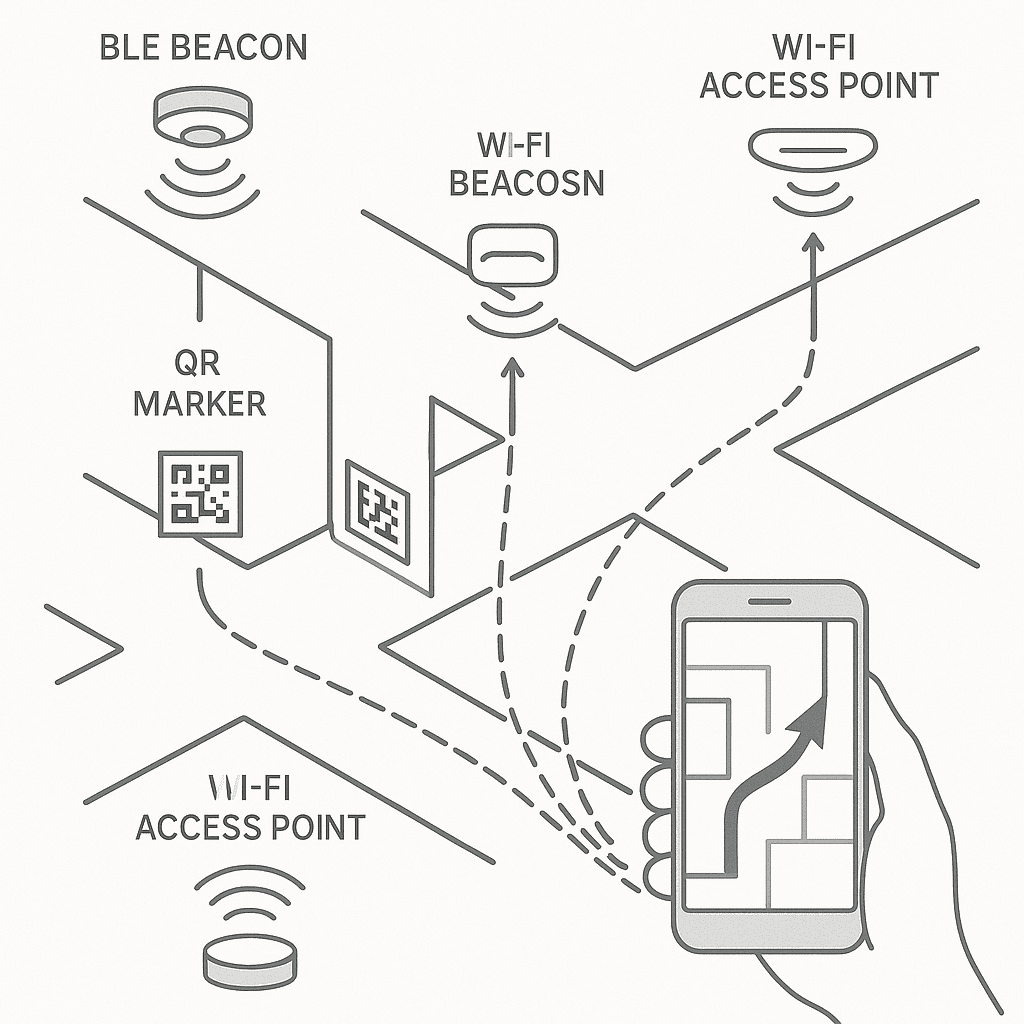
Indoor positioning
Turn-by-turn navigation inside buildings requires a positioning layer. Each approach has trade-offs:
- Bluetooth Low Energy (BLE) beacons: reliable, cost-effective, and widely supported; requires beacon placement and battery/maintenance plan.
- Wi‑Fi RTT or trilateration: uses existing Wi‑Fi infrastructure; accuracy varies with density and calibration.
- Ultra-wideband (UWB): high accuracy; higher cost and device compatibility considerations.
- QR/NFC location nodes: scan to set location at decision points; no continuous tracking, low cost and privacy-friendly.
- Magnetic field and vision-based methods: minimal hardware; success depends on device capabilities and environment.
For many clinics, a hybrid approach is pragmatic: QR codes at key points combined with mobile web navigation provide guidance without deploying a full positioning network on day one.
Hardware considerations
- Displays: high-brightness, commercial-grade panels suitable for 16/7 or 24/7 operation; proper ventilation.
- Touch: responsive capacitive touch; optional touchless gestures for infection control contexts.
- Enclosures: robust, secure, ADA/AS 1428 compliant heights and reach; cable management; easy to clean.
- Power and network: PoE where possible for low-power devices, otherwise secure AC with UPS; wired Ethernet preferred, LTE backup for resilience.
- Environmental: glare control, minimal reflections, and adequate lighting; consider acoustic environment around kiosks.
Content management, governance, and operations
The best map is only as good as its data. To keep wayfinding trustworthy, establish clear content ownership and workflows:
Centralised content management
- Use a secure content management system (CMS) to manage destinations, routes, zones, and screens.
- Role-based access: administrators, editors (clinics), and approvers (facilities) with audit trails and versioning.
- Scheduled changes: plan future moves and route adjustments with automatic go-live dates.
- Emergency override: publish alerts, detours, or evacuation messaging across relevant screens instantly.
Operational processes
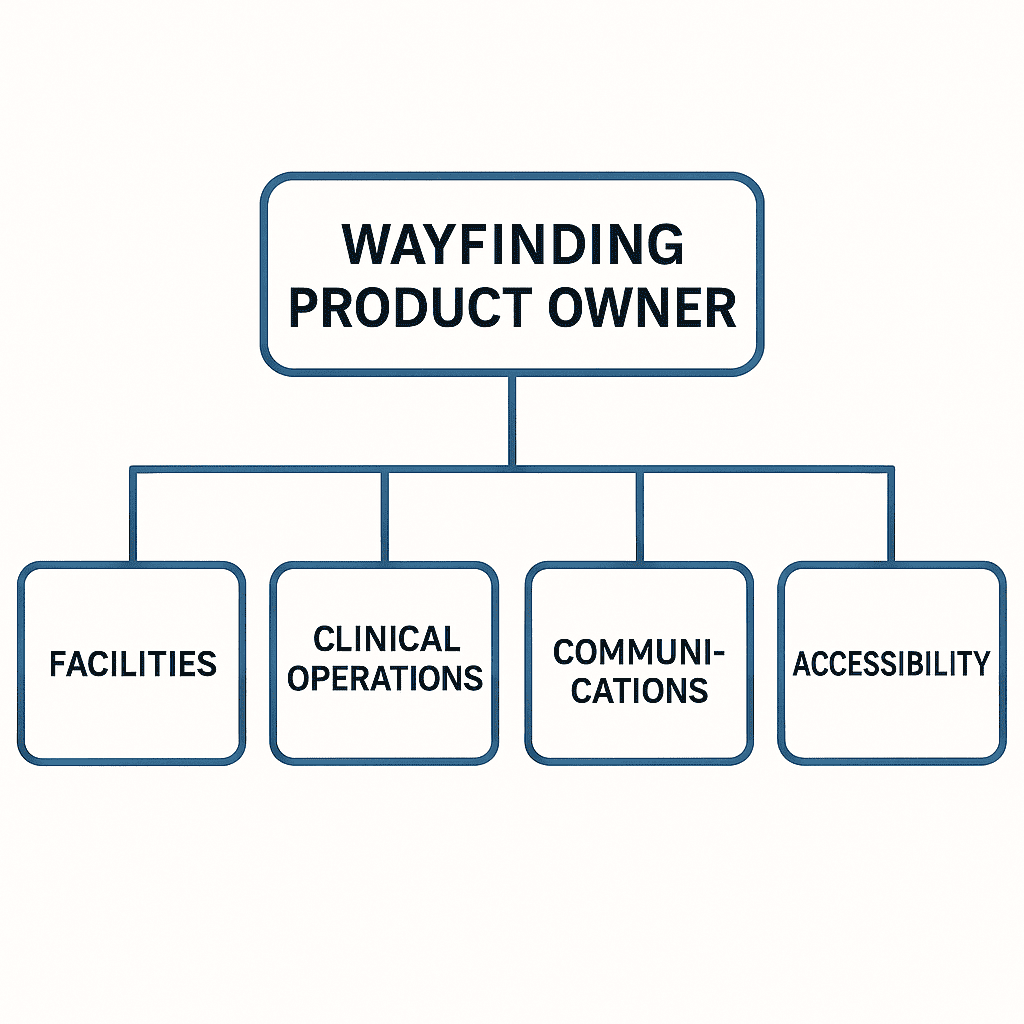
- Governance: a cross-functional steering group (facilities, clinical operations, communications, accessibility) meets regularly.
- Change intake: clinics submit updates via a simple form; facilities review for accuracy and impact.
- Quality assurance: test routes after any structural change; validate step-free options.
- Monitoring: uptime and health of devices, content sync status, and beacon network checks.
- Maintenance: cleaning regimes, screen calibration, and scheduled hardware refresh cycles.
Training and adoption
- Staff orientation: reception and volunteers learn to help visitors use kiosks and share route links.
- Communications: posters and digital signs announce the system; QR codes on appointment letters invite pre-visit planning.
- Feedback loops: quick surveys on kiosks and mobile help refine search terms, synonyms, and landmarks.
Privacy, security, and safety
Healthcare environments demand rigorous attention to privacy and security. While wayfinding systems typically do not process clinical information, they still collect and handle data that must be protected.
Privacy by design
- Minimise personal data: avoid collecting identifiable information for standard wayfinding use.
- Anonymous analytics: gather aggregated usage metrics (e.g., searches for destinations) without tracking individuals.
- Transparent notices: clear privacy statements on kiosks and mobile maps; opt-out for any optional features.
- Comply with the Australian Privacy Principles (APPs) and relevant health privacy legislation.
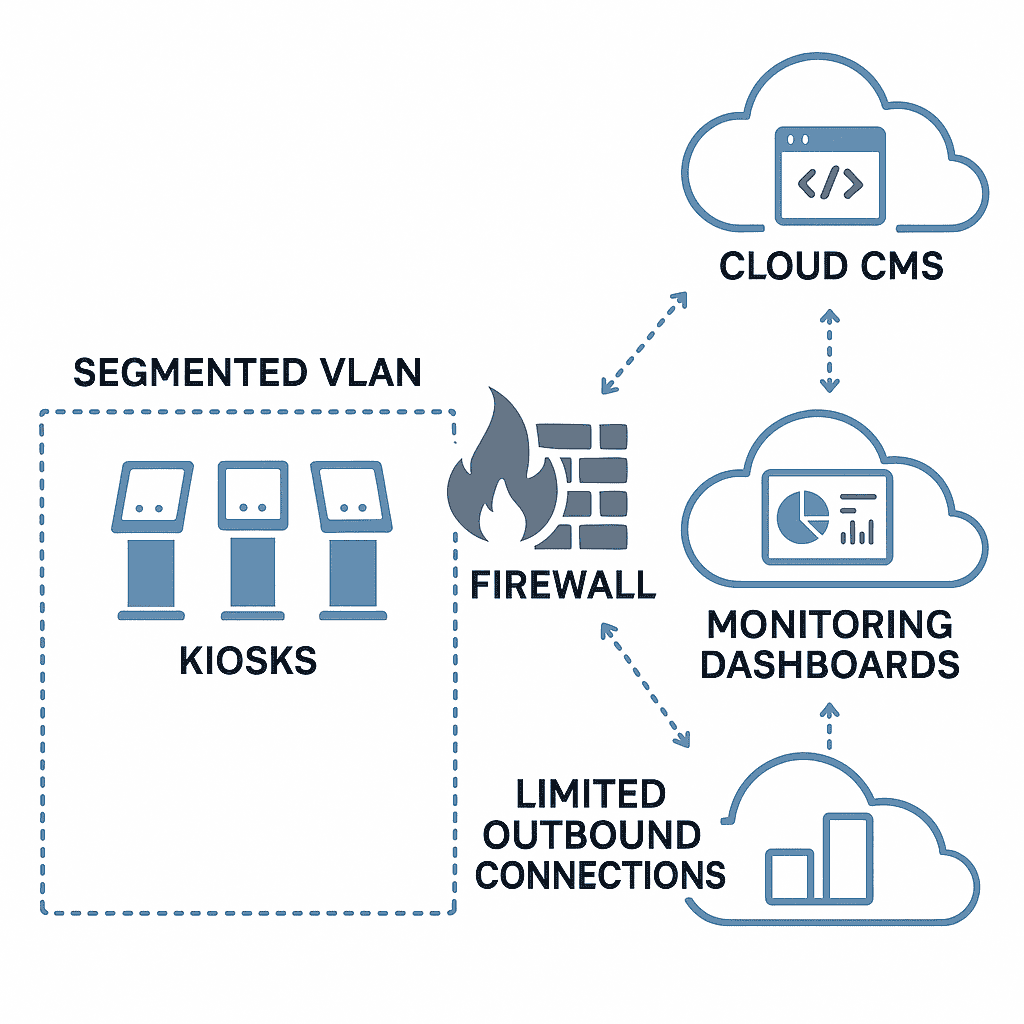
Security best practices
- Device hardening: kiosk mode, application whitelisting, blocked OS-level gestures, and locked enclosures.
- Network segmentation: isolate wayfinding devices from clinical networks; restrict outbound traffic to required services.
- Patching and updates: regular OS and application updates; monitored remotely with secure MDM.
- Penetration testing and vulnerability management as part of the organisation’s security programme.
- Backup and recovery: CMS and map data backed up; documented disaster recovery procedures.
Safety and compliance
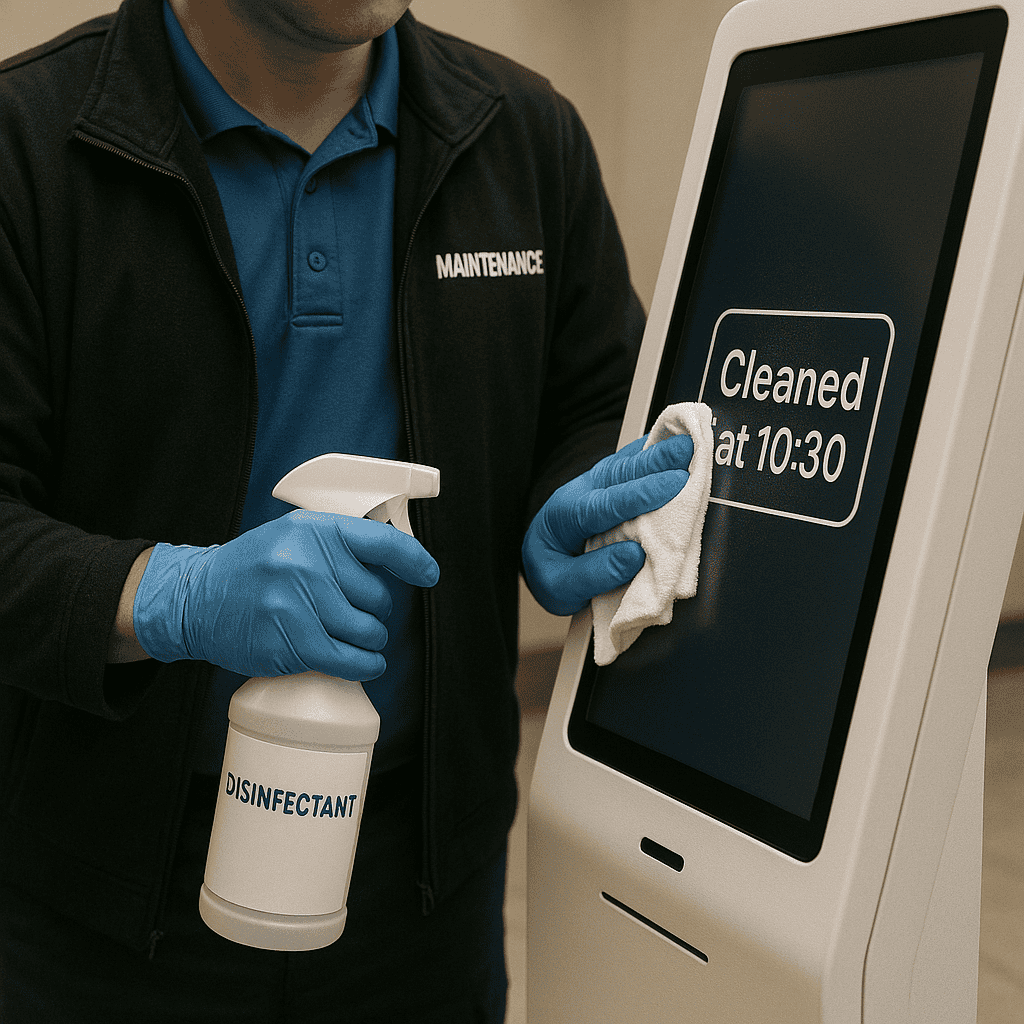
- Infection control: antimicrobial screen coatings where appropriate; defined cleaning protocols for high-touch surfaces.
- Accessibility compliance: kiosk heights, reach ranges, and clear floor space aligned with AS 1428 requirements.
- Emergency messaging: ability to display critical information while ensuring safety protocols remain clear and authoritative.
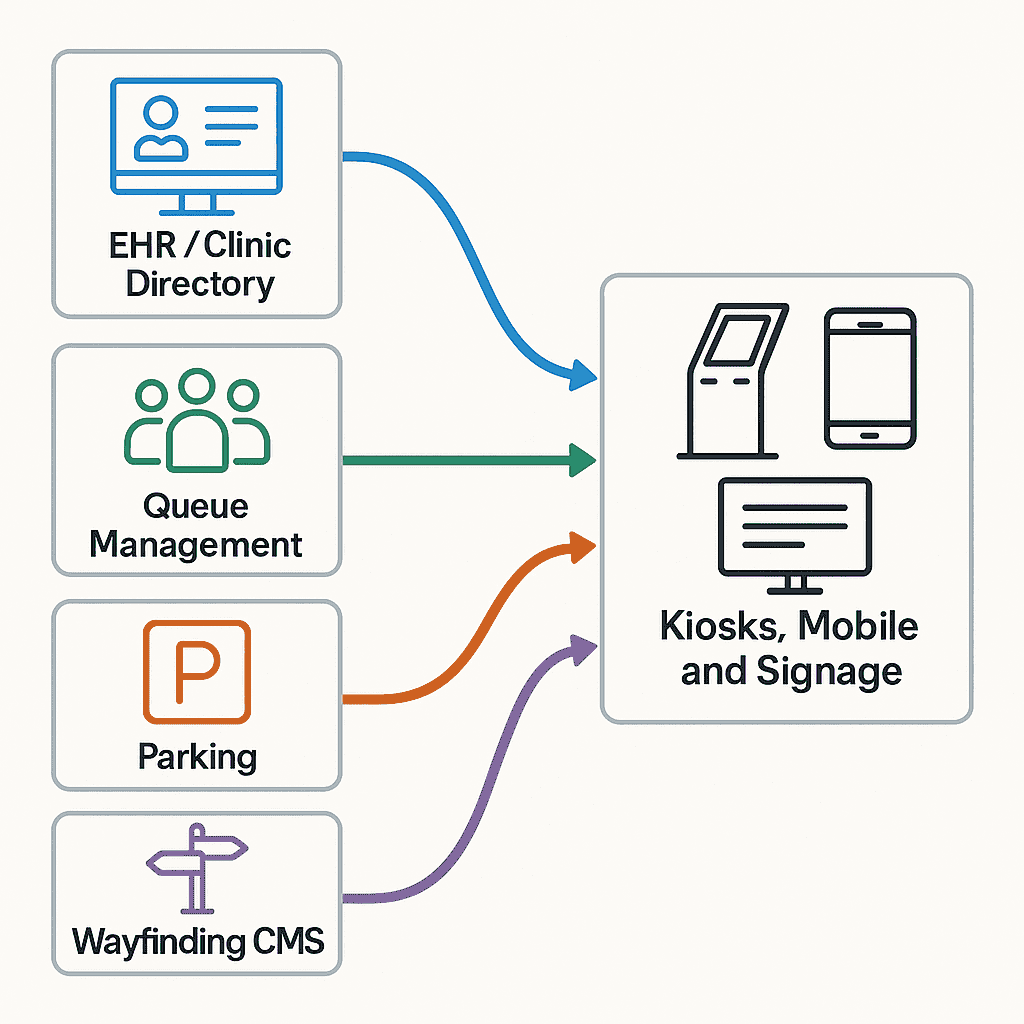
Integrations that make the experience seamless
Digital wayfinding becomes more powerful when it connects with the systems that run your centre:
- Clinic directories and scheduling: import clinician lists, specialties, and suite numbers; sync changes from source-of-truth systems.
- Appointment reminders: include deep links to precise destinations; trigger “I’m on my way” arrival planning.
- Queue management: direct patients to reception desks or sub-waiting areas; update routes if a clinic relocates on the day.
- Parking systems: fetch live occupancy and payment links; surface accessible bay locations.
- Building operations: reflect lift outages, corridor closures, or maintenance schedules in routing logic.
- Digital signage networks: coordinate content across directory boards, lobbies, and clinic-level screens.
- Identity and intranet: staff-facing shortcuts with single sign-on for service updates and internal maps.
Implementation roadmap: from vision to go-live
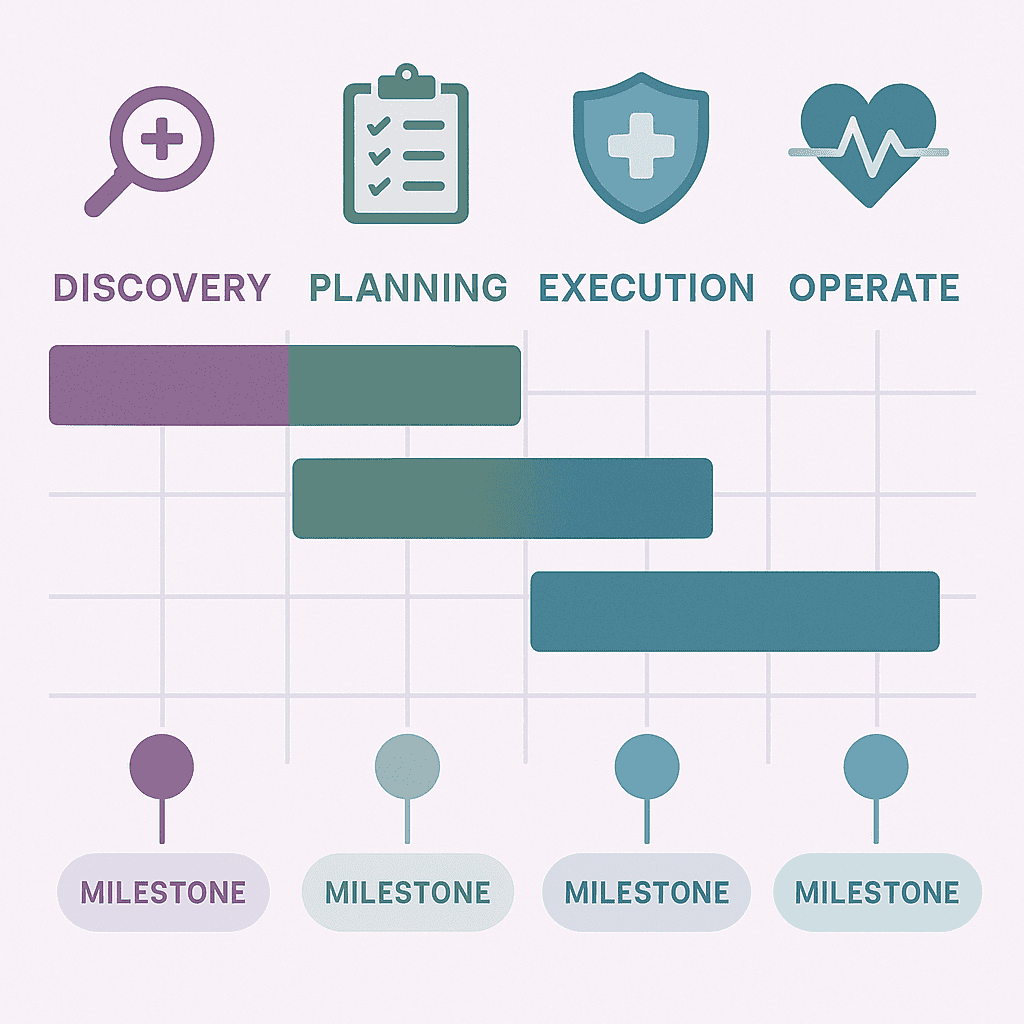
A successful deployment follows a clear pathway and respects the lived realities of your facility. Here is a typical roadmap:
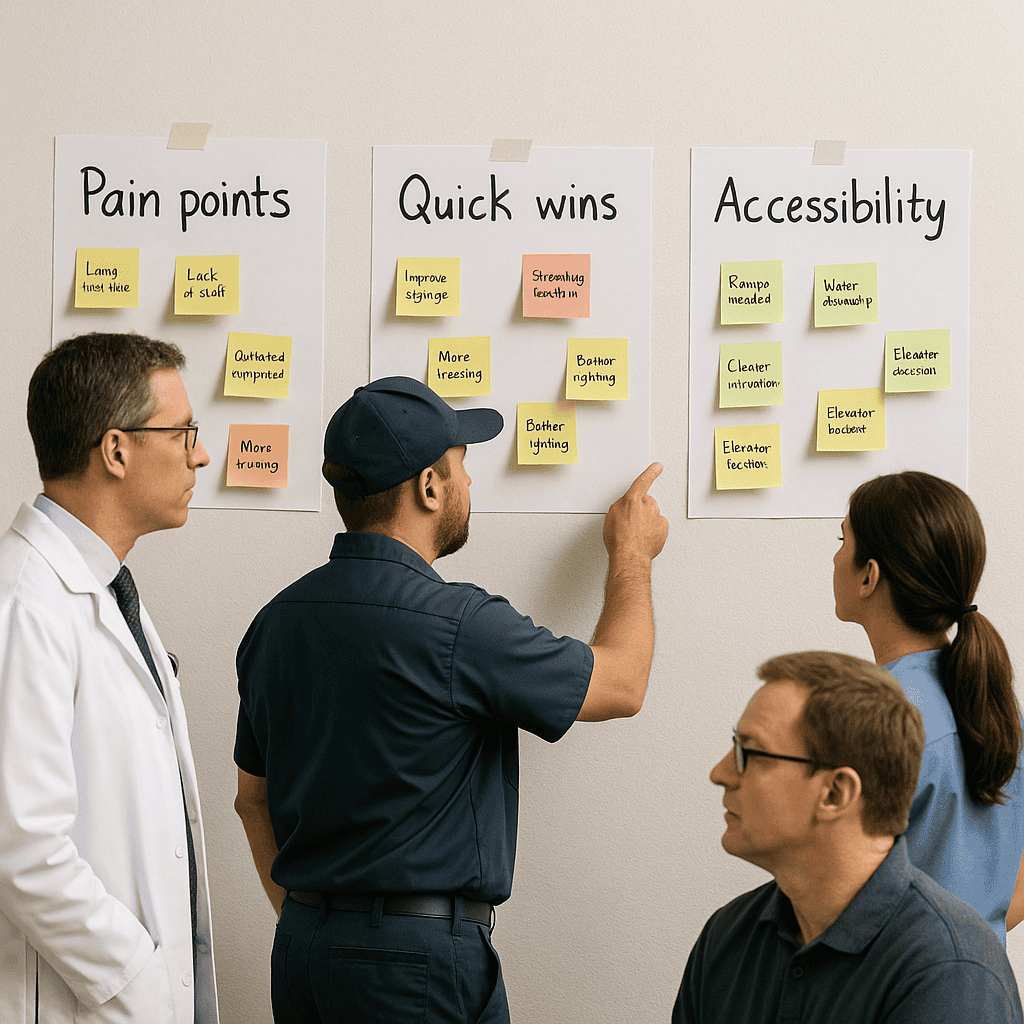
1) Discovery and alignment
- Stakeholder workshops: gather needs from facilities, clinics, reception, volunteers, accessibility specialists, and patients.
- Audit: review current signage, maps, naming conventions, and pain points (e.g., common directions asked).
- Define outcomes: set Experience, Accessibility, Operational, and ROI goals to guide decisions.
2) Information architecture and mapping
- Destination catalogue: create the canonical list with metadata and synonyms.
- Zoning: define or rationalise zone colours and codes; align with existing signage where possible.
- Base maps: produce accurate, legible floor plans optimised for both overview and step-by-step views.
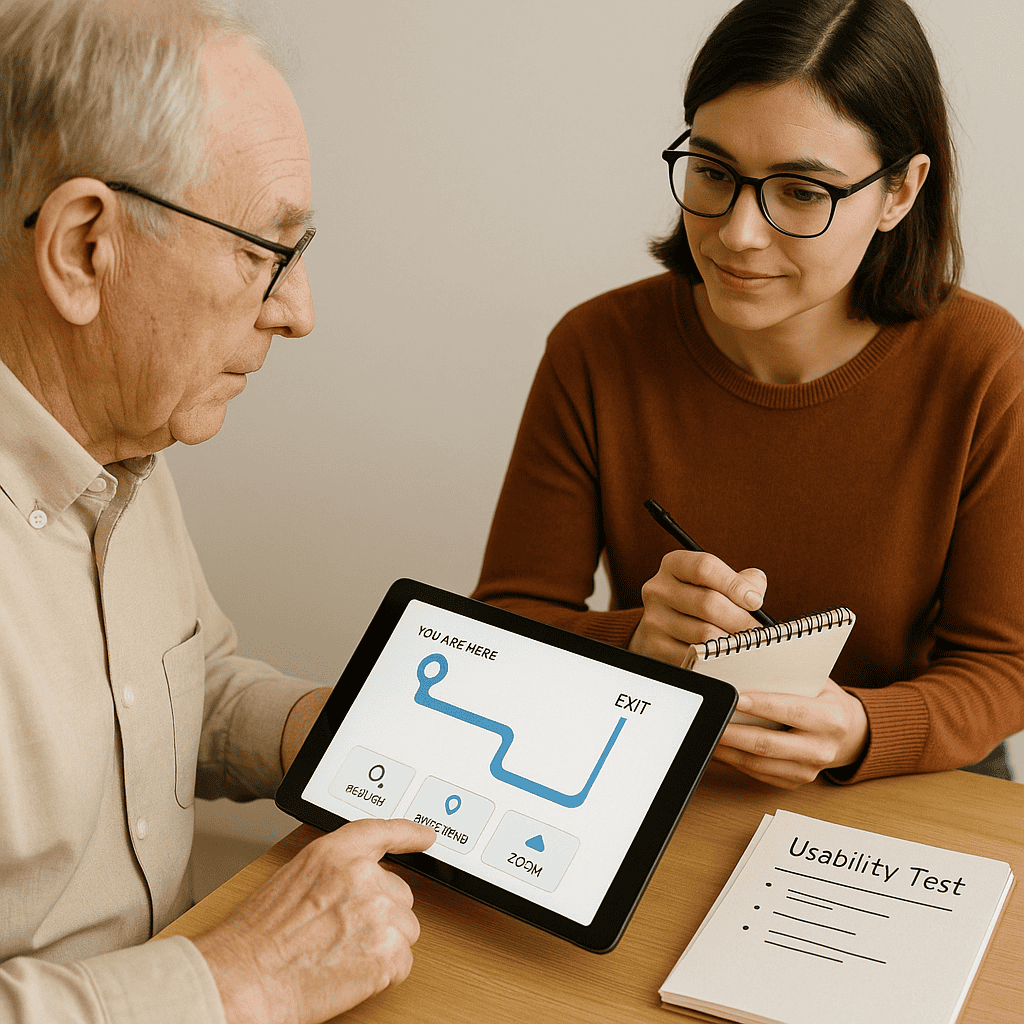
3) Prototyping and usability testing
- Interactive prototypes: test search, results, and route clarity with real users (patients and staff).
- Accessibility reviews: validate contrast, touch targets, and step-free routing; incorporate feedback.
- Iterate: refine taxonomy, icons, and route instructions based on testing insights.
4) Build and integrate
- Configure the CMS and map layers; set roles and workflows.
- Develop integrations to clinician directories, scheduling, and parking where applicable.
- Select and prepare hardware: kiosks, directory screens, mounting, power/network, and enclosures.
5) Pilot and refine
- Deploy a pilot in a defined area (e.g., main lobby and one wing).
- Measure usage, common searches, and help requests; tweak search synonyms and routes.
- Fix gaps: add missing landmarks, clarify decision points, and adjust signage if needed.
6) Rollout and training
- Scale to additional entrances, floors, and buildings in phases.
- Train reception, volunteers, and clinic staff; supply quick guides and FAQs.
- Launch communications: posters, digital displays, appointment emails, and intranet updates.
7) Operate and improve
- Monitor device health and content freshness.
- Review analytics monthly; prioritise enhancements to search and routes.
- Report outcomes to leadership and stakeholders; celebrate wins and share stories.
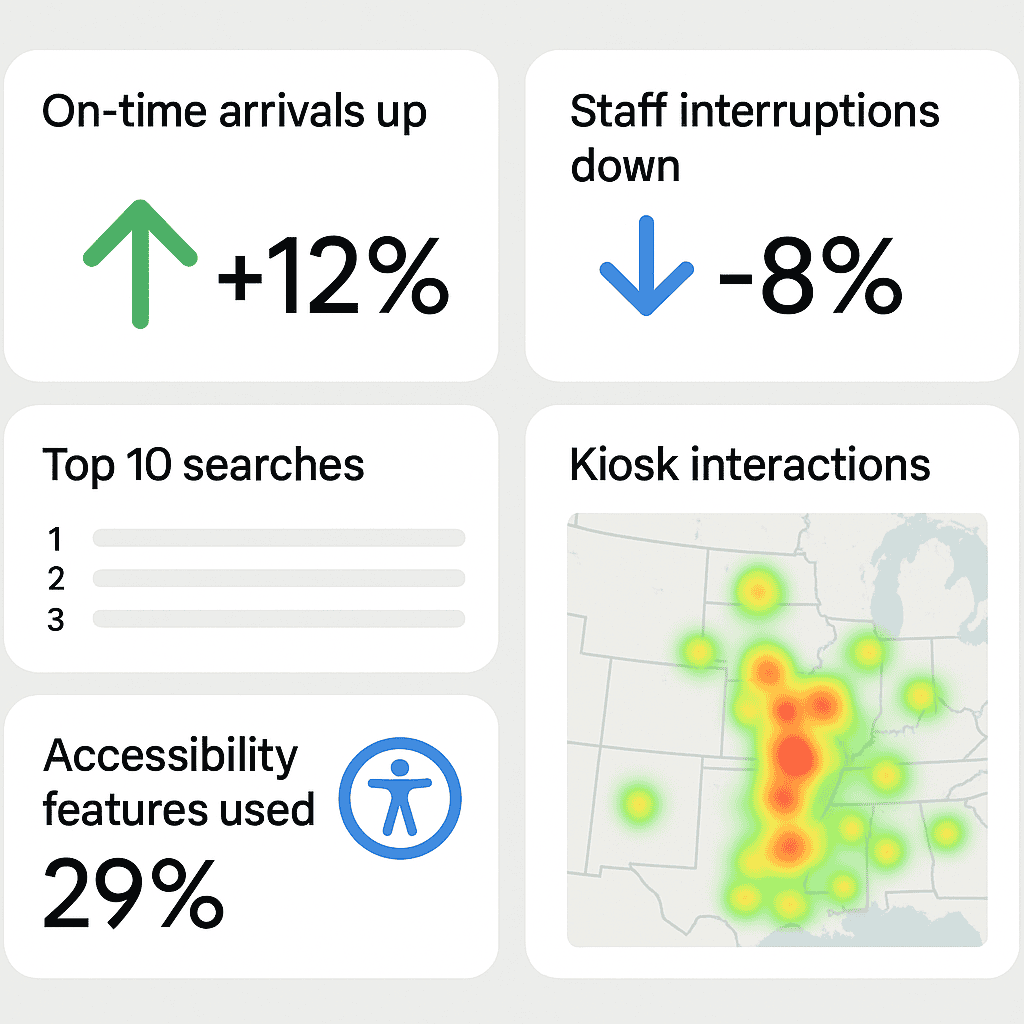
Measuring success and demonstrating ROI
Leaders need to see outcomes. While the human benefits of reduced stress are significant, you can also quantify operational impact:
Key performance indicators
- Punctuality: change in on-time arrival rates after deployment.
- Staff interruptions: reduction in “directions asked” at reception and clinics.
- Search success: percentage of searches resulting in a route started.
- Completion: route start-to-finish rates (for mobile sessions).
- Accessibility usage: uptake of step-free routes, language toggles, and text-to-speech.
- Operational agility: time from announcement of a closure to live detour on screens.
Cost and benefit categories
- Costs: hardware, software licences, CMS configuration, integrations, installation, training, support.
- Benefits: time saved by staff, reduced late arrivals, fewer missed appointments, improved patient satisfaction, lower print costs, faster response to changes.
You can also tell a qualitative story: fewer confused visitors in corridors, calmer waiting rooms, or volunteers reporting easier conversations. These lived experiences are persuasive alongside the numbers.
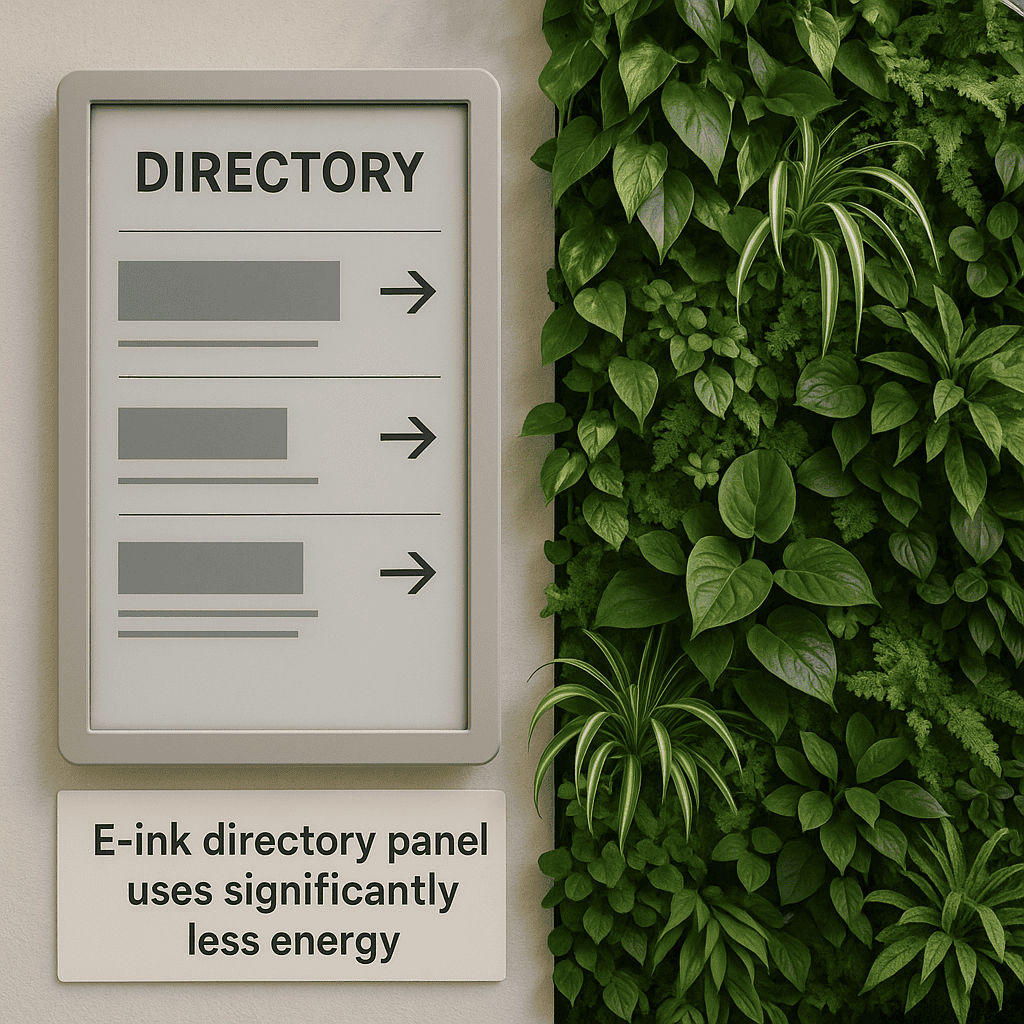
Sustainability and lifecycle thinking
Medical centres are rightly focused on sustainability and responsible procurement. Wayfinding can contribute:
- Reduce paper waste by replacing frequently outdated print maps with dynamic digital guidance.
- Choose energy-efficient displays and schedule off-hours dimming or sleep modes where appropriate.
- Consider e-ink for low-change areas (e.g., clinic directories) to minimise energy use.
- Adopt modular hardware that supports component replacement rather than full unit disposal.
- Plan for responsible e-waste handling and secure data sanitisation at end of life.
Common pitfalls—and how to avoid them
- Ignoring the taxonomy: without a clear destination catalogue and synonyms, search fails and frustration grows.
- Underestimating change management: staff need to know how and why to use the system; leaders must champion it.
- Inconsistent naming: mismatched terms between signs, letters, and digital maps lead to conflicting directions.
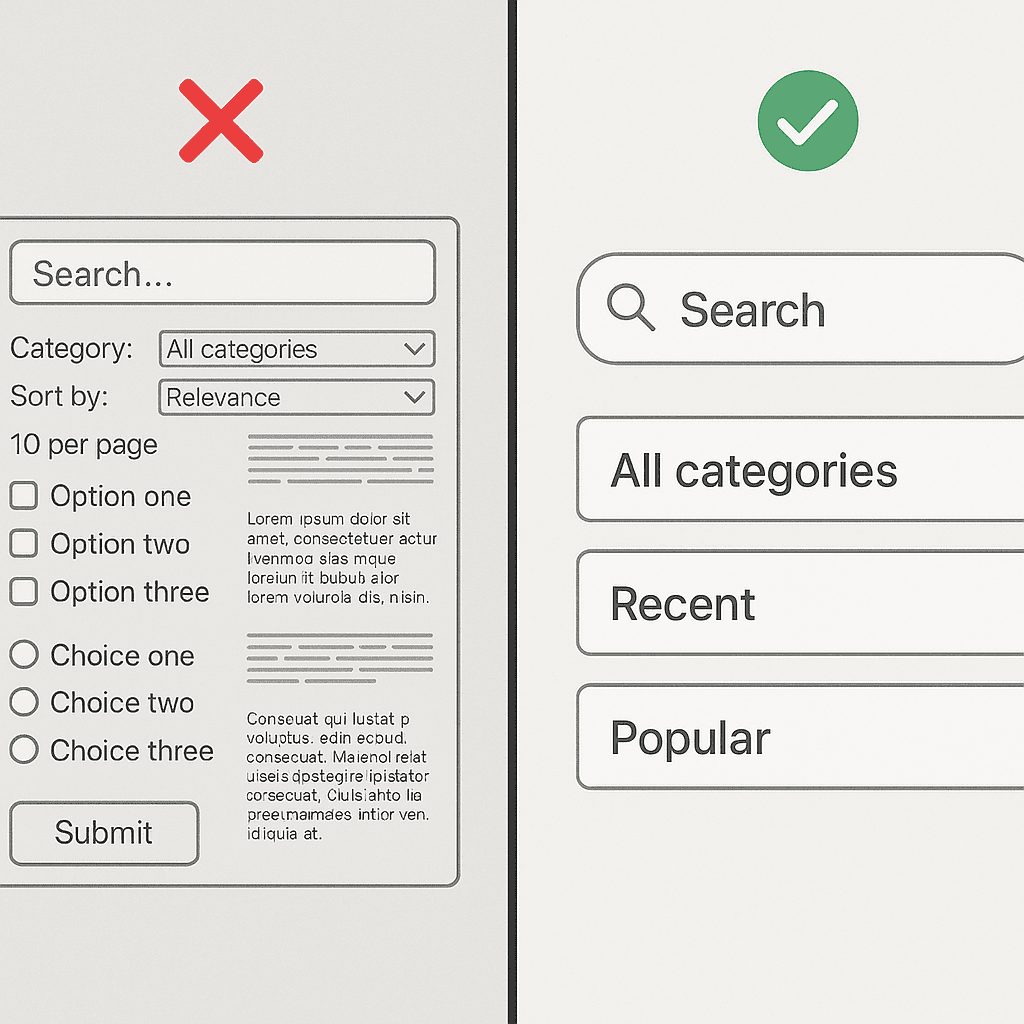
- Overcomplicating the UI: too many options create decision paralysis; prioritise the common journeys.
- Neglecting accessibility: if step-free routes, large text, or audio guidance are an afterthought, trust erodes.
- Letting content drift: stale directories and outdated routes break confidence; assign clear ownership.
- Infrastructure oversight: poor Wi‑Fi, insufficient power, or glare-prone placements limit effectiveness.
- Vendor lock-in: prefer open standards and exported data to maintain long-term flexibility.
Future trends worth watching
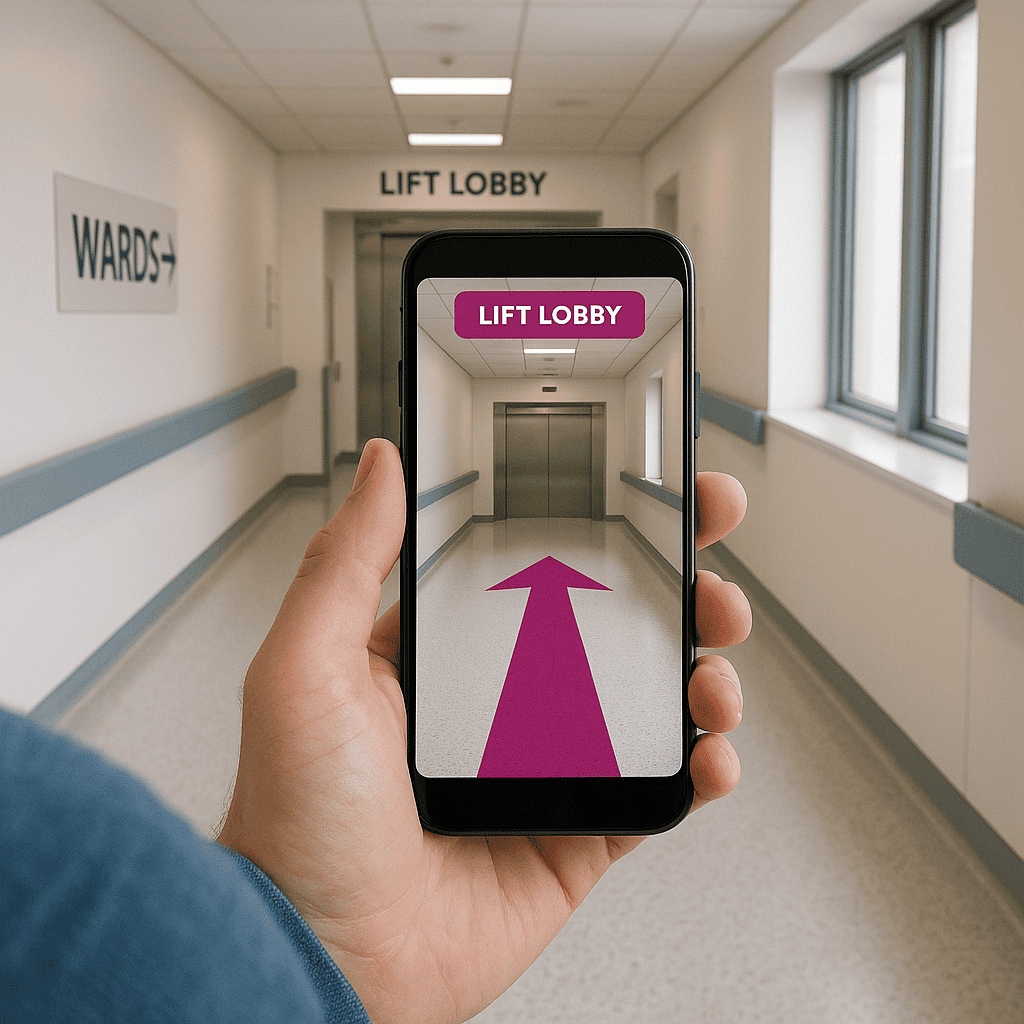
- AR-assisted navigation: camera overlays to show arrows in corridor views for those who prefer visual cues.
- Contextual personalisation: routes that adapt to appointment timing, mobility preferences, and known constraints.
- Digital twins: facility models that synchronise with operational data to simulate flows and plan detours.
- Voice interfaces: hands-free search and directions on kiosks and mobiles with noise-aware microphones.
- Open mapping standards: interoperable map data that can be reused across apps and systems securely.
Case study highlight: MRS480 Specialist Centre
Digital Wayfinding Solutions has implemented healthcare wayfinding across a range of environments. In our MRS480 Specialist Centre project, we delivered a tailored digital wayfinding solution for a busy, multi-tenant specialist clinic setting. The approach focused on clear zoning, clinician-focused search, accessible routes, and a content governance model that keeps information accurate as clinics evolve. You can read the case study here: MRS480 Specialist Centre digital wayfinding solution.

Designing routes that people actually follow
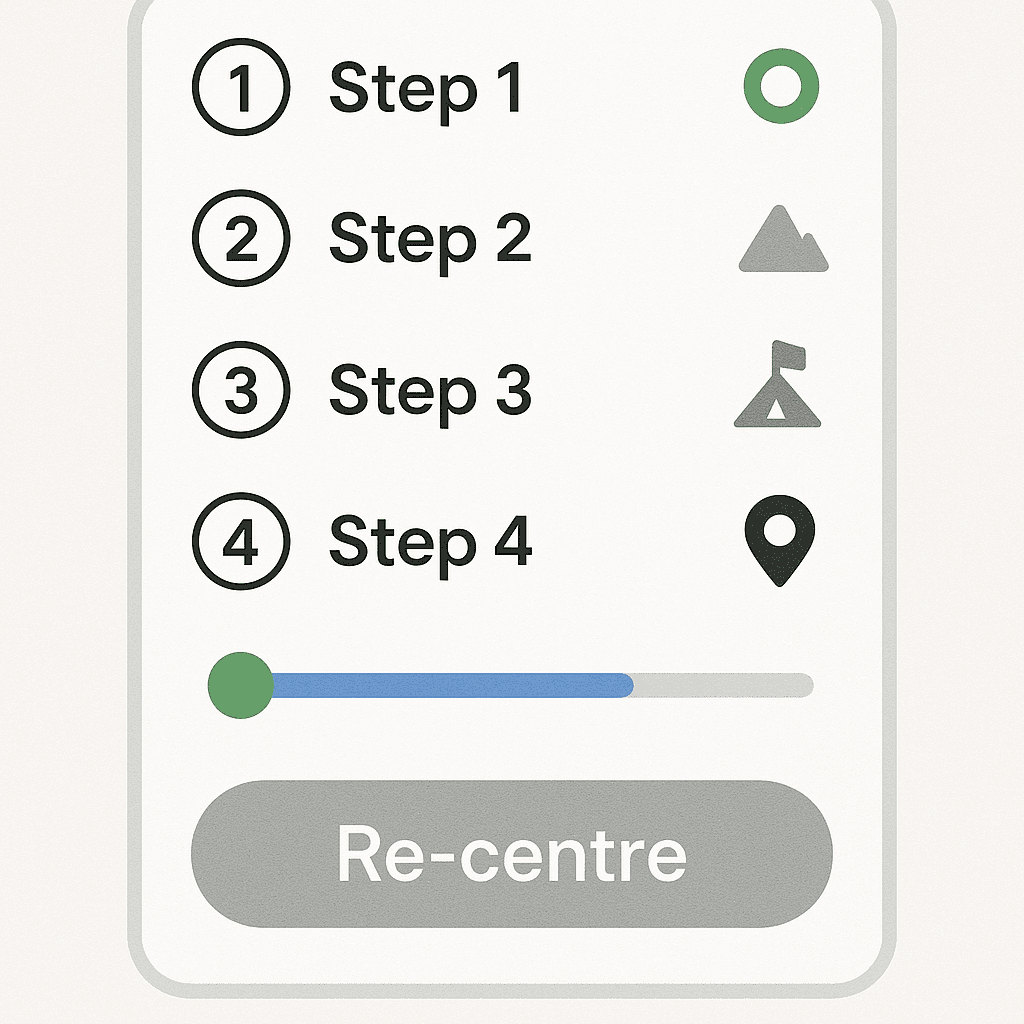
A route is more than a line on a map. Consider what helps someone stay confident as they move:
- Step count and time: show a realistic time estimate and number of steps or distance.
- Decision points: preview turns and lift changes; clearly label “G” vs. “LG” vs. “1” (ground versus first storey).
- Landmarks: “Pass the pharmacy” adds reassurance between turns.
- Progress markers: “You’re halfway there” messages reduce anxiety.
- Re-orientation: allow quick re-centre and “nearest help desk” prompts if the user strays off-route.
- Return journey: make “back to entrance” or “back to car park” one tap away at all times.
Naming that works in the real world
Language is powerful. In healthcare, naming must be accurate and human. Tips:
- Prefer patient-friendly names: “Children’s Imaging” in addition to “Paediatric Radiology.”
- Maintain a synonym library: “X-ray”, “Medical Imaging”, “Radiology” all resolve to the same place.
- Show both clinician and clinic names: “Dr Sarah Ahmed (Endocrinology) – Suite 3.14, Zone B.”
- Don’t rely on acronyms alone: spell out the meaning in results and signage.
- Localise languages for the community you serve; consult with cultural liaison teams for accuracy and tone.
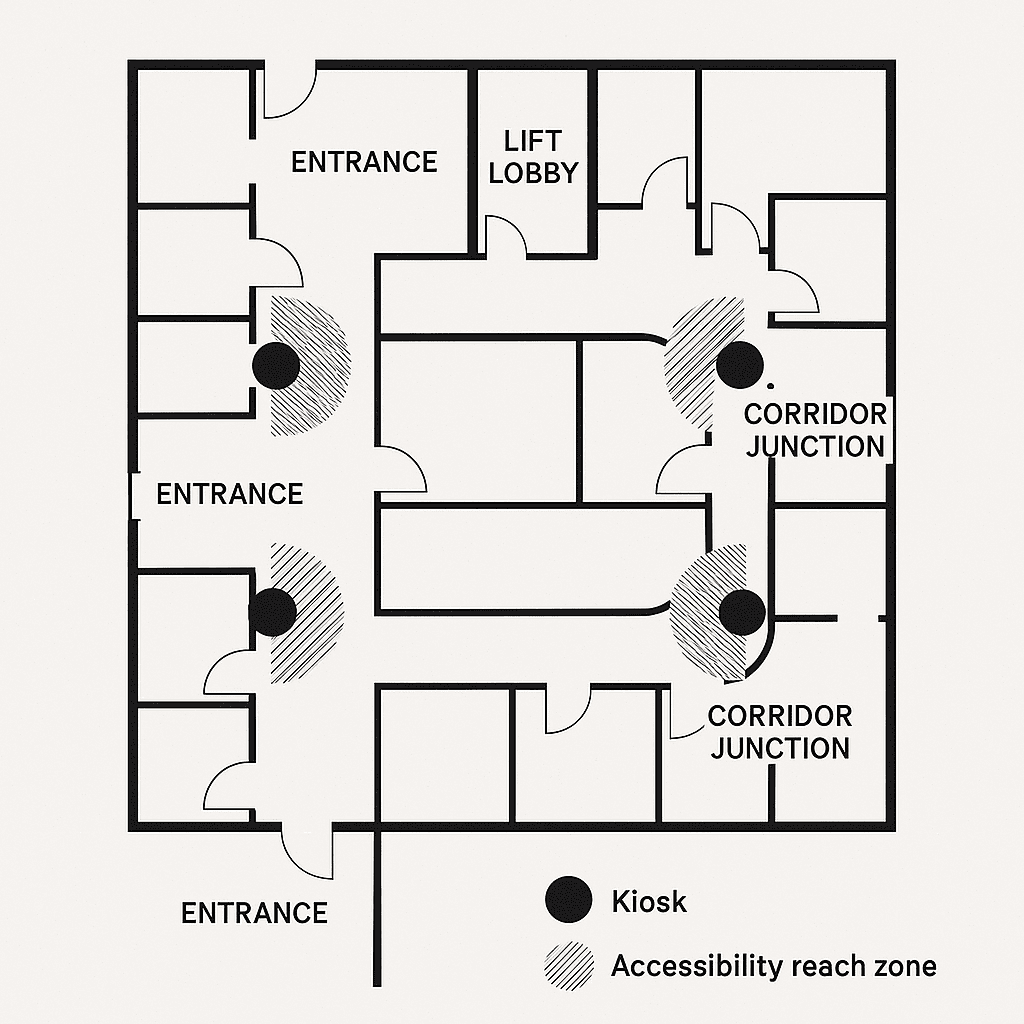
Placement and ergonomics: where screens belong
Even the best interface fails if the kiosk is hidden or physically awkward. Plan placements to align with real footfall and sightlines:
- Entrances and lobbies: first touchpoint with adequate space to step aside and plan.
- Decision points: at corridor junctions and lift lobbies where routes branch.
- Eye-line and reach: mounts at heights that meet accessibility reach ranges, with clear floor space for wheelchair users.
- Glare and noise: avoid direct sunlight; place away from loud HVAC or echo-prone corners to aid audio guidance.
- Redundancy: ensure at least two kiosks near main entrances to handle peak loads and maintenance windows.
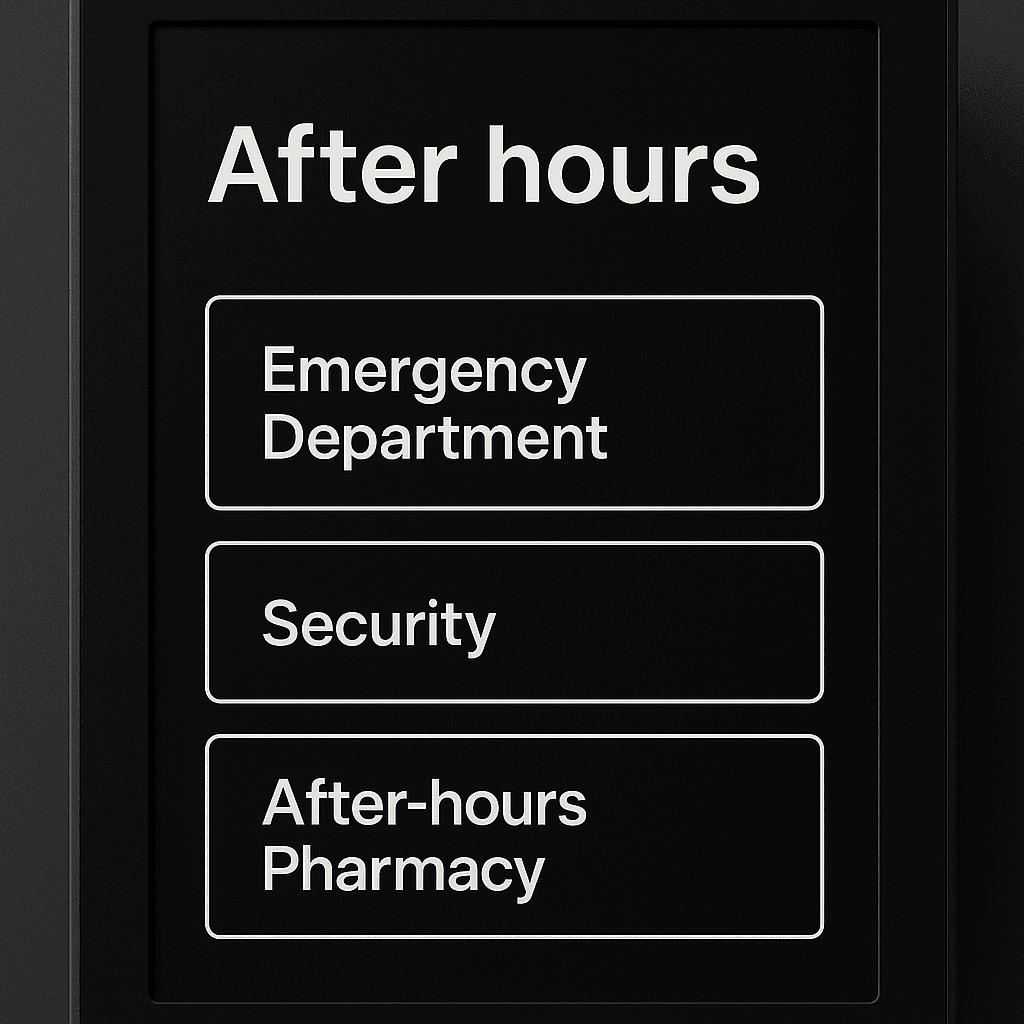
Emergency, after-hours, and resilience modes
Medical centres operate beyond 9–5, and the unexpected happens. Build resilience and responsive modes:
- After-hours mode: strip to essential routes (e.g., ED, Security, After-hours Pharmacy), dim screens appropriately.
- Emergency messaging: pin critical alerts with clear formatting; ensure overrides are controlled and logged.
- Offline gracefully: cache maps and routes; show essential directions if the network drops.
- Power continuity: UPS for kiosks and network gear; plan for safe shutdowns and auto-recovery.
Cleaning, durability, and infection control
Infection control requirements shape hardware and maintenance choices:
- Use enclosures and touch surfaces compatible with approved cleaning agents; provide cleaning guidance to staff.
- Minimise crevices and exposed cables; choose sealed designs where possible.
- Consider touchless options (voice or gesture) for specific contexts, with accessible alternatives.
- Schedule regular cleaning and calibration; record in maintenance logs for accountability.
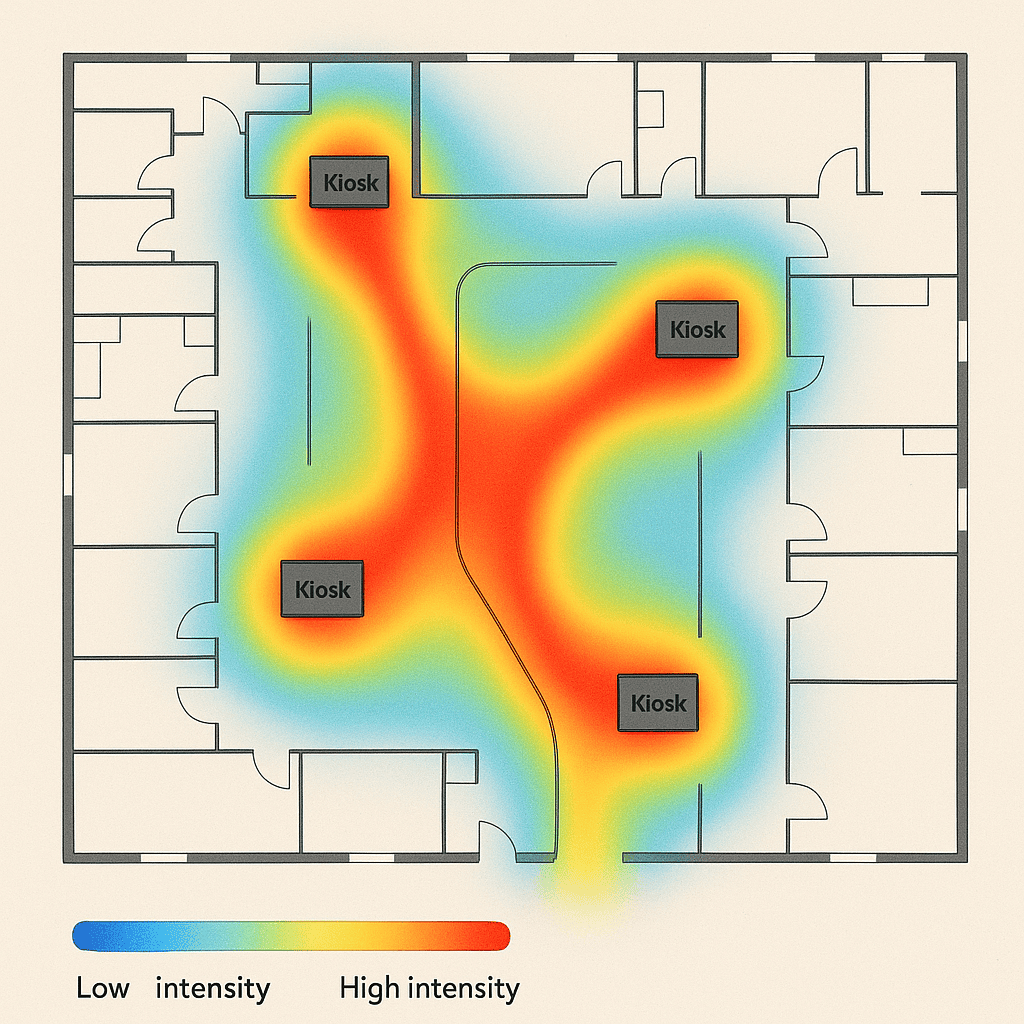
Analytics that inform operations and design
Anonymous analytics can guide better decisions without compromising privacy:
- Top searches: reveal which clinics and clinicians are most in demand; ensure they are easy to find.
- Null searches: identify missing synonyms or new destinations that need adding.
- Route drop-offs: see where users abandon a route to review clarity or signage alignment.
- Kiosk heatmaps: optimise placements and plan for additional units where demand is high.
- Accessibility usage: understand how often step-free routes and language toggles are used to prioritise improvements.
Governance framework and ownership
Clear accountability makes the system sustainable:
- Executive sponsor: champions the programme, removes roadblocks, and secures funding.
- Product owner (facilities or digital): accountable for outcomes, roadmap, and vendor management.
- Editors (clinics/receptions): propose updates to destinations and opening hours.
- Approvers (facilities/communications): validate changes and ensure consistency.
- Accessibility lead: audits new features and reviews changes for inclusive design.
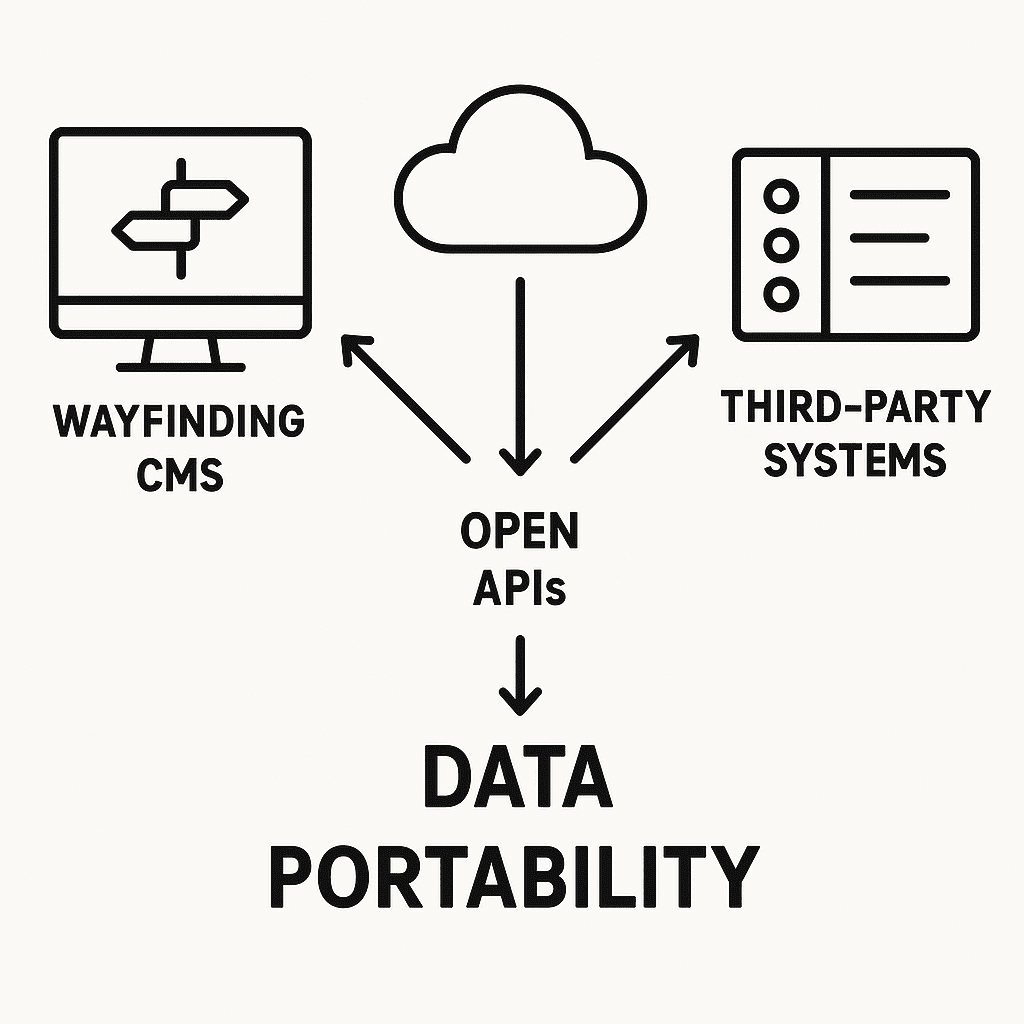
Interoperability and avoiding lock-in
Choose platforms that keep you in control of your data and future choices:
- Map and destination data export: ensure you can export in common formats for reuse and backup.
- Open APIs: integrate with appointment systems, parking, and signage without proprietary lock-in.
- Standards alignment: where available, align with emerging indoor mapping standards to future-proof investments.
- Modular procurement: separate hardware from software when appropriate to allow upgrades over time.
Practical checklist: are you ready to start?
- We have a cross-functional team (facilities, clinics, communications, accessibility) ready to collaborate.
- We can provide or validate accurate floor plans.
- We have a list of clinics, clinicians, and destinations—even if it needs rationalisation.
- We understand our common visitor journeys and pain points.
- We can allocate owners for content updates and approvals.
- We know our preferred kiosk locations, power, and network constraints.
- We have clarity on accessibility requirements and languages for our community.
- We have objectives and KPIs to measure success.

Frequently asked questions
Do we need indoor positioning for turn-by-turn navigation?
Not always. Many centres start with interactive kiosks and mobile web maps using decision-point guidance and QR codes. If your building has long, similar corridors and complex junctions, positioning (e.g., BLE beacons) can add confidence. You can phase this in later.
How long does implementation take?
Timelines depend on scale and integrations. A focused pilot in a single building lobby can go live in a few weeks after discovery. A campus-wide rollout with integrations and multiple kiosks typically spans several months, including testing and training.
What about people who prefer print?
Digital wayfinding complements, not replaces, static signage. Offer printed route slips at kiosks and ensure static signs align with digital naming and zone colours.
Can we update content ourselves?
Yes. A good CMS provides role-based editing and approvals so facilities and clinic staff can keep information accurate without vendor tickets for every change.
Is it accessible?
It should be. Ensure your solution meets WCAG 2.2 AA, supports screen readers or text-to-speech on kiosks, offers large text, step-free routing, and multiple languages. Validate with accessibility experts and real users.
How do we handle temporary changes or construction?
Publish time-bound detours in the CMS so routes update automatically. Align with facilities’ maintenance schedules and communicate changes via digital signage and pre-visit messages.
How is data privacy handled?
Collect only what you need. Use anonymous analytics, provide clear privacy notices, and align with the Australian Privacy Principles. Avoid storing sensitive personal health information in the wayfinding system.
What’s the expected lifespan of hardware?
Commercial displays and kiosks typically last 5–7 years with proper maintenance. Choose modular hardware so components like media players can be refreshed without replacing enclosures.
Can we integrate with our appointment reminders?
Yes. Add deep links that open precise destinations in the web map, with options for accessible routes, parking, and public transport info.
How do we measure success?
Track punctuality, staff interruptions, search success rates, route completions, and accessibility feature uptake. Pair quantitative metrics with qualitative feedback from staff and patients.
From confusion to confidence: your next step
Digital wayfinding turns a complex medical centre into an environment that feels navigable and humane. It respects people’s time and reduces stress at moments when clarity matters most. It also pays operational dividends, freeing staff to focus on care.
If you are exploring digital wayfinding for your medical centre, review our healthcare work and consider the practical steps outlined in this guide. You can see an example of our approach in the MRS480 Specialist Centre case study.

Appendix: sample content patterns that work
Search categories
- Clinician: name, specialty, consulting suite.
- Clinic/department: “Cardiology Clinic”, “Pathology Collection”.
- Procedure: “ECG”, “MRI”, linked to the right location and prep info.
- Amenity: toilets, café, chapel, baby change, pharmacy.
- Administrative: billing, medical records, enquiries.
Route instruction style
- Start: “From Main Entrance (Blue Zone), head straight 20 metres towards the café.”
- Turn: “At the café, turn right and follow signs to Lift Bank B.”
- Lift: “Take the lift to Level 3 (Third storey).”
- Final: “Exit the lift, turn left. Cardiology Reception is ahead on your right.”
Accessibility cues
- “Step-free route” badge on routes that avoid stairs.
- “Quiet route” option avoiding busy corridors where feasible.
- Rest points highlighted every 50–80 metres where seating exists.
Conclusion
Digital wayfinding for medical centres is both a design discipline and an operational practice. It demands clarity of language, sensitivity to people, and a resilient technology foundation. When these elements align, centres see calmer arrivals, more punctual clinics, and a measurable reduction in daily friction. Most importantly, patients and families feel supported at every step.
To discuss how a digital wayfinding solution could fit your centre, including pilots, integrations, and accessibility planning, get in touch with the team behind the MRS480 Specialist Centre implementation at Digital Wayfinding Solutions.